July – December 2020
Following declarations from the US Department of Health and Human Services and World Health Organization ending the COVID-19 Public Health Emergency, the IARS COVID-19 Scientific Advisory Board (SAB) concluded its review of the scientific literature about SARS-CoV-2 in August. The SAB has reviewed more than 3,100 journal articles and published 1,076 article reviews over the past 42 months. It has been an enormous commitment from the SAB, and the IARS owes our dedicated physician volunteers a huge debt of gratitude for their unwavering participation in this initiative.
To search by keyword, select Ctrl + F on a PC and Command + F on a Mac. Then, enter keyword and Enter.
The material on this website is provided for informational purposes and does not constitute medical advice. New knowledge is added daily and may change over time. Opinions expressed should not be construed as representing IARS policy or recommendations. References and links to third parties do not constitute an endorsement or warranty by IARS.
Retractions:
- Effectiveness of Surgical and Cotton Masks in Blocking SARS–CoV-2: A Controlled Comparison in 4 Patients – published on April 6, 2020 in the Annals of Internal Medicine, retracted on June 1, 2020.
- Hydroxychloroquine or chloroquine with or without a macrolide for treatment of COVID-19: a multinational registry analysis – published in The Lancet on May 22, 2020, subjected to an expression of concern on June 2, and retracted on June 4.
- Cardiovascular Disease, Drug Therapy, and Mortality in Covid-19 – published in the New England Journal of Medicine on May 1, 2020, subjected to an expression of concern on June 2, and retracted on June 4.
December 18, 2020:
- Baricitinib plus Remdesivir for Hospitalized Adults with Covid-19. 12/11/20. Kalil AC. N Engl J Med.
This article provides the encouraging outcome of a randomized trial enrolling 1033 patients in 8 countries, led by the team that conducted ACTT-1, the remdesivir randomized control trial. The oral anti-inflammatory drug baricitinib, a selective inhibitor of Janus kinase (JAK) 1 and 2, in combination with remdesivir, proved safe and superior to remdesivir alone for the treatment of hospitalized patients with COVID-19. While the primary outcome, time to recovery, improved by one day only, patients with impending respiratory failure benefitted most with progression to death or invasive ventilation being 31% lower in the combination group. The discussion includes a detailed review of the drugs’ potential dual action as an anti-inflammatory and antiviral and makes a pertinent comparison with dexamethasone and the RECOVERY trial.
The incidence of side effects of JAK inhibitors (immunosuppression, secondary infections, and thrombosis) were not significantly higher when baricitinib was added. - Evidence of thrombotic microangiopathy in children with SARS-CoV-2 across the spectrum of clinical presentations. 12/8/20. Diorio C. Blood Adv.
This study, designed for researchers, examined 50 COVID-19 pediatric hospitalized patients for soluble C5b9 and thrombotic microangiopathy. C5b9 were found to correlate with the severity of disease and serum creatinine. Thrombotic microangiopathy was found in 17 of the 19 patients examined. These data help characterize COVID-19 disease in the pediatric population and help form the building blocks for further study. - On the whereabouts of SARS-CoV-2 in the human body: A systematic review. 10/30/20. Trypsteen W. PLOS Pathogens.
This article is a well-presented review of available literature through June 2020. The strength of this paper resides in its focus on viral presence and evidence of replication and infectivity in different organ systems. It acknowledges the fact that the presence of an ACE2 receptor does not control viral cell entry per se. It concludes that while we have a good understanding of the presence and replication mechanisms in the respiratory system, a full understanding of the underlying mechanism of organ toxicity – direct viral, micro-vascular or inflammatory – in other systems (heart, kidney, CNS) remains inconclusive.
December 16, 2020:
- Decontamination and Reuse of N95 Filtering Facepiece Respirators: Where Do We Stand? 12/15/20. Cassorla L. Anesth Analg.
Interest in decontamination methods for N95 respirators increased during the COVID-19 pandemic along with shortages and altered practices in health care facilities. This is a well-referenced review of available science. Best-supported methods are based upon time, heat, microwave-generated steam, hydrogen peroxide, or UV-C (ultraviolet germicidal irradiation, UVGI). Many require special equipment and most require procedures to prevent cross-contamination and return each respirator to its original user due to the potential for residual organisms other than SARS-CoV-2. Tables include reference websites, a summary of methods, and current FDA emergency use authorizations. - Feasibility and Safety of Prone Position Transport for Severe Hypoxemic Respiratory Failure Due to Coronavirus Disease 2019. 12/9/20. Seethala RR. Crit Care Explor.
This is a retrospective review of 25 COVID-19 patients, transported and ventilated while prone from outlying hospitals to tertiary medical centers in Boston. Using ground transportation with a median transport time of 38 minutes, and specially trained nurse and paramedic critical care teams, this transport agency developed a protocol to transport prone patients. These patients were quite sick, with a median intubation duration of 5 days before transport. The condition of the patients, the protocols, and events during transport are carefully documented. All patients successfully arrived at their destination. This study provides evidence that when carefully implemented, prone transport may be safe and facilitate otherwise impossible transfers for potentially life-saving tertiary care. - Prevalence and prognostic value of elevated troponins in patients hospitalised for coronavirus disease 2019: a systematic review and meta-analysis. 12/9/20. Zhao BC. J Intensive Care.
Elevated troponin levels on admission were linked to a higher risk of death in patients admitted for COVID-19. This retrospective article of worldwide reports demonstrated a 20.8% elevated troponin concentration at admission resulting in a 42% mortality vs. 9% in those admitted with normal levels. Mortality was not linked to cardiac deaths, but included deaths from all causes suggesting that troponin might indicate infectious-related injury beyond the heart. The article is extremely deep in the description of data collection and evaluation making for a difficult read. 51 studies were included for the review. - Update: Characteristics of Symptomatic Women of Reproductive Age with Laboratory-Confirmed SARS-CoV-2 Infection by Pregnancy Status — United States, January 22–October 3, 2020. 11/6/20. Zambrano LD. MMWR Morb Mortal Wkly Rep.
In a CDC analysis of 409,000 women aged 15–44 with symptomatic, laboratory-confirmed COVID-19 and known pregnancy status, pregnancy (n=23,434) notably increased the risk of ICU admission, invasive ventilation, ECMO, and death. Pregnancy status was reported in 35.5% of women with COVID-19 during the study period. Compared with non-pregnant women, adjusted risk ratios were 3.0 for ICU admission, 2.9 for invasive ventilation, 2.4 for ECMO, and 1.7 for death, a mortality of 1.5 per 1000. Hispanic, Black and older pregnant women had even greater risks of death. All pregnant women should be counseled on the additional importance of precautions against SARS-CoV-2 infection.
The material on this website is provided for informational purposes and does not constitute medical advice. New knowledge is added daily and may change over time. Opinions expressed should not be construed as representing IARS policy or recommendations. References and links to third parties do not constitute an endorsement or warranty by IARS.
Retractions:
- Effectiveness of Surgical and Cotton Masks in Blocking SARS–CoV-2: A Controlled Comparison in 4 Patients – published on April 6, 2020 in the Annals of Internal Medicine, retracted on June 1, 2020.
- Hydroxychloroquine or chloroquine with or without a macrolide for treatment of COVID-19: a multinational registry analysis – published in The Lancet on May 22, 2020, subjected to an expression of concern on June 2, and retracted on June 4.
- Cardiovascular Disease, Drug Therapy, and Mortality in Covid-19 – published in the New England Journal of Medicine on May 1, 2020, subjected to an expression of concern on June 2, and retracted on June 4.
December 14, 2020:
- Association between statin use and outcomes in patients with coronavirus disease 2019 (COVID-19): a nationwide cohort study. 12/5/20. Butt JH. BMJ Open.
This study utilized the Danish public health record system to disprove claims of a June 2020 published observational study from China which found a relative risk reduction in mortality of 42% among COVID-19 inpatients receiving statins.
In a tightly controlled cohort study, recent statin exposure did not influence all-cause mortality of severe SARS-CoV-2 infection. Theories of a cardio-protective, anti-inflammatory or immune-response modulating mechanism could not be substantiated. - Cardiac complications in patients hospitalised with COVID-19. 11/23/20. Linschoten M. Eur Heart J Acute Cardiovasc Care.
This article shows results from a 3011 patient multi-national/institutional study designed to determine the role of cardiovascular (CV) disease in COVID-19 patients admitted to the hospital enrolled between April and June. Eleven and a half percent (349) of the patients had CV complications with AF 4.7% (142) being the most common. Eight hundred thirty-seven patients required ICU/high dependency unit, of which 87% required mechanical ventilation; overall mortality was 19.8%. Patients with pre-existing cardiac disease (ischemia, heart failure) were more likely to develop complications. Pulmonary embolism was reported in 6.6% of patients overall but was found in 18.9% of those who were admitted to the ICU. These results suggest that elevated troponin levels in absence of electro- or echocardiography abnormalities should be interpreted cautiously and may more likely be related to demand ischemia. The authors conclude that incidence of cardiac complications during hospital admission is low, despite frequent patient histories of pre-existing cardiovascular disease.
SAB Comment: This article highlights difficulty in diagnosing primary cardiac complications from biomarkers alone. While not diagnostic, elevated troponin levels have been associated with increased mortality in COVID-19 patients as well as in other ARDS-associated conditions (e.g. septic shock, post-traumatic injury). - Right ventricular dysfunction in critically ill COVID-19 ARDS. 11/26/20. Bleakley C. Int J Cardiol.
Interesting observational study/retrospective analysis of RV echocardiographic data collected on 90 patients requiring invasive ventilation revealed that RV dysfunction was under-diagnosed with long axis views of the RV. Analysis noted radial measurement of RV dysfunction correlated with elevations in hs-Tn1 and NT pro-BNP, indicators of myocardial injury possibly related to high afterload. The authors suggest a new phenotype of RV dysfunction in COVID-19 not seen in other ARDS diagnoses. Of note, 42% of patients were receiving vino-venous ECMO. The authors suggest that findings that indicate hyperdynamic results on longitudinal views may represent a response to radial dysfunction. Excellent descriptions and tables are included.
December 11, 2020:
- Association of inhaled and systemic corticosteroid use with Coronavirus Disease 2019 (COVID-19) test positivity in patients with chronic pulmonary diseases. 12/4/20. Liao SY. Respir Med.
This study of 928 patients tested at National Jewish Health respiratory hospital for COVID-19 found 113 (12%) were positive. Retrospective analysis showed that using inhaled corticosteroids was not associated with a change in the likelihood of testing positive for COVID-19. Being treated with systemic corticosteroids was actually associated with a slight decrease in the likelihood of testing positive for COVID-19, especially in patients with chronic pulmonary disease or airway diseases (asthma or COPD). - Characteristics of Adults aged 18-49 Years without Underlying Conditions Hospitalized with Laboratory-Confirmed COVID-19 in the United States, COVID-NET – March-August 2020. 12/3/20. Owusu D. Clin Infect Dis.
This article describes a Center for Disease Control-funded, cross-country study of non-pregnant adults younger than 50 years old providing the causes of hospital admissions due to COVID-19. While fever was a common presenting symptom, the illness primarily affected the pulmonary system. 22% were admitted to ICU although death occurred in <1%. 74% of patients were male and authors discuss the possibility of genetics linked to ACE2 receptor as a cause of infection severity.
Of note, 42% of patients were Hispanic/Latino; treatment was not controlled; obesity and the use of steroids were not reported; 20% of patients were healthy prior to infection; 12% received remdesivir. - Controversies in airway management of COVID-19 patients: updated information and international expert consensus recommendations. 12/1/20. Wei H. Br J Anaesth.
This editorial by a panel of international experts summarizes the COVID-19 airway management literature on the effectiveness of personal protective equipment (PPE), transmission of the virus during high flow nasal oxygen therapy (HFNO), and the debate over early vs. late intubation. Tables nicely summarize the examined literature. Their consensus includes:- The higher the PPE level, the better the protection.
- There is no convincing evidence that HFNO increases the risk of COVID-19 cross-infection to healthcare workers.
- Timing of intubation will depend upon individual pathophysiology, the trajectory of the illness, and the response to trials of noninvasive airway management.
- More study is needed.
- COVID-19 Associated Thrombosis and Coagulopathy: Review of the Pathophysiology and Implications for Antithrombotic Management. 11/24/20. Ortega-Paz L. J Am Heart Assoc.
This is a comprehensive, well-written, albeit lengthy, review of COVID-19 pathophysiology and therapies. Cardiovascular, thrombotic, and coagulopathic manifestations are emphasized along with the importance of individual risk assessment for venous thromboembolism (VTE). Multiple validated VTE risk assessment tools are enumerated. A theory of imbalanced ACE/ACEII receptors as a risk factor for SARS-CoV-2 infection is discussed. Useful summary figures and tables include knowledge gaps and ongoing areas of research. - Pulmonary embolism in COVID-19 patients: Prevalence, predictors and clinical outcome. 12/3/20. Scudiero F. Thromb Res.
This retrospective database study from 7 Italian hospitals looked over the echocardiogram results of 224 patients with COVID-19 of whom 14% had PE confirmed by CTA. The purpose was to identify which echocardiographic findings best predict pulmonary embolism. PE patients were hospitalized a longer time after symptom onset, showed higher D-dimer level and a higher prevalence of myocardial injury. At multivariable analysis, tricuspid annular plane systolic excursion (TAPSE) and systolic pulmonary arterial pressure were the only parameters independently associated with PE. Mortality rates (50% vs 27%; p = 0.010) and cardiogenic shock (37% vs 14%; p = 0.001) were significantly higher in PE patients. - The ADAMTS13-von Willebrand factor axis in COVID-19 patients. 11/23/20. Mancini I. J Thromb Haemost.
This study examines the VWF antigen to ADAMTS13 activity ratio in 50 COVID-19 hospitalized patients and demonstrates that this ratio was strongly associated with COVID-19 severity. Three groups of patients were studied, namely those receiving nasal oxygen, CPAP treatment, or intubation with ventilatory support. The authors suggest that these data represent potential new markers of disease severity and further support the concept of micro thrombogenesis in patients with severe COVID-19.
SAB Comment: This is new scientific information to help understand pathophysiology of micro thrombosis but routine ADAMTS13 testing isn’t recommended. - Tobacco use as a well-recognized cause of severe COVID-19 manifestations. 11/30/20. Gupta AK. Respir Med.
Though we have reviewed articles, some saying that COVID-19 is worse in smokers and others that it is not, the authors reviewed 23 articles that met their criteria. The authors noted that pre-existing comorbidities in tobacco users such as cardiovascular diseases, diabetes, respiratory diseases, and hypertension are found to further aggravate the disease manifestations. More generally, smoking is a potential risk factor for, not only contracting the viral infection, but also making the treatment of such COVID-19 patients more challenging.
December 7, 2020:
- Early Percutaneous Tracheostomy in Coronavirus Disease 2019: Association With Hospital Mortality and Factors Associated With Removal of Tracheostomy Tube at ICU Discharge. A Cohort Study on 121 Patients. 11/17/20. Rosano A. Critical Care Medicine.
This single-center Italian study reviewed outcomes of 121 COVID-19 patients treated with early percutaneous tracheostomy between 4 and 12 days (median 6) following ICU admission. Includes detailed discussion of rationale, inclusion criteria, methods, decannulation strategies and rehabilitation. Outcomes include procedural safety and efficacy for providers and patients, ability to decannulate survivors in ICU and trend to improved survival. Also discussed are improved/earlier weaning, and easier management and discharge from ICU. A useful comparison with other relevant studies is provided. - Early Percutaneous Tracheostomy During the Pandemic “As Good as It Gets”. 11/19/20. Auzinger G. Critical Care Medicine.
This related editorial discusses percutaneous tracheostomy risk/benefit related to COVID-19 as well as other ICU conditions including ARDS and MERS. Strengths of the related article, the largest single-center study of percutaneous tracheostomy for COVID-19 disease, include a pragmatic approach relating to timing and choice of percutaneous vs. surgical approach based on well-described protocols for management and decannulation extant prior to the pandemic. This editorial compares the study’s strengths to others in literature and notes that while early tracheostomy may be considered a risk to the procedural team, the incidence of subsequent +COVID tests in participants was lower than in other ICU staff. This editorial amplifies Rosano’s manuscript and understanding regarding timing and potential benefits of early tracheostomy in COVID-19 patients. - Loneliness, Mental Health, and Substance Use among US Young Adults during COVID-19. 10/28/20. Horigian VE. J Psychoactive Drugs.
Frequently discussed in mass media, this paper presents the psychologic issues associated with the COVID-19 pandemic. In addition, intensivists and anesthesiologists should be aware of possible alcohol and drug use intended by the patient to relieve depression associated with this illness and its treatment. - No evidence for increased transmissibility from recurrent mutations in SARS-CoV-2. 11/25/20. van Dorp L. Nat Commun.
SARS-CoV-2 is not becoming more transmissible or virulent. In jumping from animal to human, SARS-CoV-2 might evolve or adapt toward higher transmissibility. This study examined whether viral changes have emerged repeatedly and independently (homoplasies) and if repeated mutations in human lineages made the virus more transmissible. Using a 99-country dataset of 46,723 SARS-CoV-2 genomes compared to the reference Wuhan-Hu-1, investigators did not identify a single recurrent mutation convincingly associated with increased viral transmission. So far, as an endemic human pathogen, recurrent mutations appear to be evolutionary neutral, single lineage and primarily induced via RNA editing, rather than being signatures of adaptive pressure and a new separate phenotype. - Olfactory transmucosal SARS-CoV-2 invasion as a port of central nervous system entry in individuals with COVID-19. 11/30/20. Meinhardt J. Nature Neurosci.
Viral penetrance of the CNS is likely through diverse routes. These investigators demonstrate in 33 autopsies morphological changes associated with SARS-CoV-2 neurotropism, such as thromboembolic ischemic infarction of the CNS and the presence of SARS-CoV-2 RNA and protein in anatomically distinct regions of the nasopharynx and brain. By exploiting the proximity of olfactory mucosal, endothelial and nervous tissue, including olfactory and sensory nerve endings, virus can cross into the olfactory CNS. Subsequently, SARS-CoV-2 appears to penetrate other areas of the CNS, including the primary respiratory and cardiovascular control centers in the medulla oblongata. - Repurposed Antiviral Drugs for Covid-19 – Interim WHO Solidarity Trial Results. 12/2/20. WHO Solidarity Trial Consortium. N Engl J Med.
Beginning in March 2020, the WHO Solidarity trials enrolled 11,330 patients in 405 hospitals in 30 countries representing all six WHO regions and randomly assigned them to receive either remdesivir, lopinavir, hydroxychloroquine or interferon beta-1a regimens or to receive hospital-specific standard care. None of these drugs achieved the desired goal of a reduction in 28-day mortality. Except for remdesivir, all trials have since been discontinued.
SAB Comment: Despite a negative outcome, this work is encouraging as it shows WHO’s capability to direct a rigorous global study protocol and a complex data collection and report it in a timely manner. - Tissue-specific Immunopathology in Fatal COVID-19. 11/20/20. Dorward DA. Am J Respir Crit Care Med.
In eleven post-mortems these authors investigated whether inflammation is primarily a direct reaction to SARS-CoV-2 or an independent organ-specific immunopathologic reaction. Using multiplex PCR and in situ viral spike protein detection, SARS-CoV-2 organotropism was mapped. Multiple virus-independent aberrant immune responses mostly in lungs and reticuloendothelial system were found. These viral-independent immunopathologic features included monocyte/myeloid-rich pulmonary artery vasculitis, pulmonary parenchymal expansion of monocytes/macrophage-lineages and in the reticuloendothelial system, iron-laden macrophages and plasma cell responses. They concluded that a disconnect between viral presence and inflammation implicates immunopathology as a primary mechanism of organ injury in severe COVID-19.
December 4, 2020:
- A Randomized Trial of Convalescent Plasma in Covid-19 Severe Pneumonia. 11/24/20. Simonovich VA. N Engl J Med.
Convalescent plasma with a median titer of 1:3200 of total SARS-CoV-2 antibodies was administered a median of 8 days after the onset of symptoms to 228 hospitalized patients with severe COVID-19 pneumonia. Placebo was administered to 105 patients. Other therapy was not standardized. After 30 days there was no significant difference in outcome. Adverse effects of plasma transfusion could not be evaluated. This also suggests that passive immune therapy with monoclonal antibodies may not be beneficial to such a population.
SAB Comment: Other studies indicate that antibodies administered early after onset of symptoms to patients with mild disease are beneficial. - Assessment of 135,794 Pediatric Patients Tested for Severe Acute Respiratory Syndrome Coronavirus 2 Across the United States. 11/23/20. Bailey LC. JAMA Pediatr.
This is an epidemiologic, retrospective study of 135,794 patients younger than 25 years old tested for SARS-CoV-2 during the first 9 months of 2020 — 3% of the nation’s 2.5 million children — in a country-wide study of a consortium of children’s hospitals admissions. An overall low positive COVID-19 rate of 4% was found. Black, Hispanic and Asian youth were underrepresented yet produced higher positive results. Of the 5374 children testing positive, only 359 were hospitalized and 8 died. Six of the deaths had complex preexisting comorbidities.
Preexisting respiratory and cardiac morbidity was not a significant issue in those hospitalized. Endocrine, metabolic and malignancy-associated illnesses were linked to hospitalizations from COVID-19. Obesity was not defined. - Association Between ABO and Rh Blood Groups and SARS-CoV-2 Infection or Severe COVID-19 Illness: A Population-Based Cohort Study. 11/24/20. Ray JG. Ann Intern Med.
This population-based study of adults and children who had previous ABO blood group assessed, and who subsequently had SARS-CoV-2 testing found that O (adjusted odds ration 0.89) and Rh− (adjusted odds ration 0.80) blood groups may be associated with a slightly lower risk for SARS-CoV-2 infection and severe COVID-19 illness. Data came from 225,556 persons with a + PCR test for SARS-CoV-2 between 15 January and 30 June 2020 of 2,659,328 who had ABO/Rh measured during 2007-2019 in Ontario, Canada, a province with universal health care. - Dosing of thromboprophylaxis and mortality in critically ill COVID-19 patients. 11/23/20. Jonmarker S. Crit Care.
This is a retrospective analysis for 2 ICUs in Stockholm. In March, patients received low-dose LMWH and in April, all got medium- or high-doses. The baseline characteristics for these 152 COVID-19 patients were similar. For patients who received high-dose prophylaxis, 28-day mortality was lower (13.5%) compared to those who received medium dose (25.0%) or low-dose (38.8%), p = 0.02. Hazard ratio was 0.33 among those who received high-dose prophylaxis. There were fewer thromboembolic events in the high- (2.7%) vs medium- (18.8%) and low-dose thromboprophylaxis (17.9%) groups, p = 0.04. Bleeding rates were similar. - Incidence of venous thromboembolism and bleeding among hospitalized patients with COVID-19: a systematic review and meta-analysis. 11/17/20. Jiménez D. Chest.
This is a systematic review with meta-analysis of the world’s incidence of DVT, PE and bleeding with COVID-19. The paper offers a snapshot but also analyzes the data and points to the way forward. Forty-eight studies were selected with 18,093 patients with VTE in 17% (2/3 with DVT) and any bleeding event in 7.8%. The authors point out that this varies with whether VTE was detected by duplex screening or clinical diagnosis, percentage of ICU patients and the degree of anticoagulation. The authors point out the lack of optimal strategies and the need for controlled trials. - SARS-CoV-2 analysis on environmental surfaces collected in an intensive care unit: keeping Ernest Shackleton’s spirit. 11/23/20. Escudero D. Intensive Care Med Exp.
This study analyzed environmental contamination by SARS-CoV-2 of surfaces in a Spanish intensive care unit dedicated exclusively to the care of patients with COVID-19 and equipped with negative pressure of – 10Pa and an air change rate of 20 cycles per hour. None of 102 surface samples collected at different times of day over 2 weeks were positive by RT-PCR nor did any of the 237 ICU workers become infected by the virus. The ICU was cleaned with detergent and sodium hypochlorite twice daily. Authors discuss the contrast with studies sampling surfaces in other institutions. - SARS-CoV-2, SARS-CoV, and MERS-CoV viral load dynamics, duration of viral shedding, and infectiousness: a systematic review and meta-analysis. 11/19/20. Cevik M. Lancet.
This meta-analysis of 79 COVID-19 articles characterized viral load kinetics and dynamics, duration of viral RNA shedding, and viable virus shedding. Despite evidence of prolonged SARS-CoV-2 RNA shedding (mean 17 days) in respiratory samples, viable virus shedding appears to be short-lived (9 days maximum). Therefore, RNA detection cannot be used to infer infectiousness. High titers of SARS-CoV-2 RNA are detected from symptom onset to day 5 of illness, which probably explains the efficient spread of SARS-CoV-2 compared with SARS-CoV and MERS-CoV. These findings emphasize the importance of early case finding and prompt isolation.
December 2, 2020:
- Aerosol Retention Characteristics of Barrier Devices. 10/30/20. Fidler RL. Anesthesiology.
Investigators studied 6 barriers designed to protect health care professionals from potentially infectious aerosolized particles during airway interventions. Particle counters and mass spectrometry were used to evaluate particle spread following experimental aerosol generation and simulated cough. Performance varied widely, with closed devices performing best. Some increased exposure to the operator compared with no device. Addition of smoke evacuation techniques (e.g. suction) was also evaluated. All barriers should be used in conjunction with appropriate PPE.
An accompanying editorial discusses the importance of bioaerosol science to mitigate disease transmission in health care settings. Current experimental aerosol models remain imperfect surrogates for airborne viral disease transmission. Collaboration with bioaerosol scientists is lauded. - Comprehensive health assessment three months after recovery from acute COVID-19. 11/21/20. van den Borst B. Clin Infect Dis.
This is a well-performed and conducted study on 124 mild (not admitted), moderate and severe (ICU survivors) COVID-19-positive patients at 3-month follow-up. The comprehensive (anthropometric, psycho-social, exercise tolerance, frailty, social coping, PTSD, etc.) study indicates that significant abnormalities persisted in majority of patients irrespective of initial illness severity. Improvement in lung radiography was present in severe cases, but pulmonary function remained mildly depressed including decreasing pulse oximetry on 6-minute walk test. The conclusion is that COVID-19, as previously noted, presents long-term health care challenges including physical, psychological, neurologic and quality of life which could lead to significant future personal and societal health care burden. - Decline in SARS-CoV-2 Antibodies After Mild Infection Among Frontline Health Care Personnel in a Multistate Hospital Network – 12 States, April-August 2020. 11/27/20. Self WH. MMWR Morb Mortal Wkly Rep.
In this MMWR/CDC regarding 156 (median age 38, 94% female) frontline health care personnel who had a positive COVID-19 antibodies test result, 94% experienced a decline at repeat testing 60 days later and 28% sero-reverted to below the threshold of positivity. Health care workers with robust antibody responses were more likely to have a slower antibody decay. Whether the slimmer response of the antibody increases risk for reinfection remains unanswered. These results suggest that serology testing at a single point in time is likely to underestimate infection and a negative serologic test result might not reliably exclude prior infection. - Efficacy and Safety of Favipiravir, an Oral RNA-Dependent RNA Polymerase Inhibitor, in Mild-to-Moderate COVID-19: A Randomized, Comparative, Open-Label, Multicenter, Phase 3 Clinical Trial. 11/19/2020. Udwadia ZF. Int J Infect Dis.
Favipiravir is under investigation by the WHO and in use in Japan and Russia. It appears to accelerate viral shedding and has been used successfully for Influenza and Ebola.
Among 300 patients enrolled between May 15 and July 3, a significance in the difference in time to cessation of oral shedding, the primary endpoint, could not be achieved but the overall effect of the drug appeared favorable. - Estimated SARS-CoV-2 Seroprevalence in the US as of September 2020. 11/24/20. Bajema KL. JAMA Intern Med.
Residuals of 177,919 serum samples collected for non-COVID-19 tests by two US national commercial clinical labs were retested for antibodies to SARS-CoV-2. Four sets of samples from every state were tested from periods in late July to late September 2020. Seroprevalence varied from 23% for New York State to less than 1% for several states and was less than 10% for the vast majority of states. Nowhere was seroprevalence close to the 60% to 80% estimated to be necessary to achieve herd immunity. An excellent figure summarizes the results for each period in all 50 states. - Veno-venous extracorporeal membrane oxygenation allocation in the COVID-19 pandemic. 11/21/20. Murugappan KR. J Crit Care.
This is a well-researched and referenced discussion regarding appropriate allocation and utilization of VV-ECMO based on institutional practice. It includes ethical, practical and decision-maker considerations as well as preemptive end-of-life care discussions in severe cases. It introduces the concept of a “bridge to nowhere,” i.e., when the decision to prolong life mechanically has no future alternative/resolution. The article discusses the importance of clear communication between the health care team and patient/family consortium. It highlights the importance of clear understanding of ethical and practical implications of initiation and utilization of a scarce resource.
November 30, 2020:
- Clinical characteristics and day-90 outcomes of 4244 critically ill adults with COVID-19: a prospective cohort study. 10/29/20. COVID-ICU Group on behalf of the REVA Network and the COVID-ICU Investigators. Intensive Care Med.
In this multi-center (149 ICUs) European cohort study, the results of 4244 COVID-positive patients admitted 02/25-05/04 with ICU and 90-day follow-up were reported; ARDS severity, ventilator management and outcome at 90 days. Detailed demographic information, ventilator management, laboratory findings, ICU LOS, additional interventions and 90 day outcome reported. Overall mortality was 31% with a decrease in overall mortality noted during study; mortality was higher in older, immunocompromised, obese, diabetic patients and those with increasing ARDS severity. Higher mortality was noted in patients with shorter time between first symptoms and ICU admission. - Delirium in Older Patients With COVID-19 Presenting to the Emergency Department. 11/19/20. Kennedy M. JAMA Netw Open.
Delirium at presentation occurred in 28% of patients older than 65 years presenting to 7 US Emergency Departments. In this retrospective chart review, a total of 817 patients (mean age 78) with COVID-19 were analyzed and 16% presented with delirium as a primary symptom. Associated conditions and multivariant risk factors were identified, and impaired consciousness was listed as the predominant symptom occurring in 54% of patients with a delirium diagnosis. Delirium as a leading symptom is frequently underreported but associated with adverse outcomes and hence an important marker for poor patient outcomes (ICU stay, intubation and hospital death). - Immunomodulation as Treatment for Severe COVID-19: a systematic review of current modalities and future directions. 11/20/2020. Meyerowitz EA. Clin Infect Dis.
This current review of COVID-19 therapeutics stresses approaches to immune dysregulation and its evolving role in severe disease. Distinct early innate responses (first 5-7 days) and later adaptive immune responses must be recognized and treated accordingly. Antiviral treatment alone may be insufficient. To date, only dexamethasone shows a mortality benefit in randomized control trials when used later in the course. Late infectious and other steroid complications may be underreported. Various immunomodulatory strategies including early use of Janus kinase (JAK) inhibitors to rebalance the JAK-STAT pathways and Type I interferons are discussed. Promising early data are summarized for emerging therapies. - SARS-CoV-2 has displaced other seasonal respiratory viruses: results from a prospective cohort study. 11/15/20. Poole S. J Infect.
This is a study performed in a county in South East England on the English Channel coast of viral PCR results of tests done from March through May on patients with respiratory symptoms in the emergency department or acute care ward in most of years from 2015 through 2020. Before 2020, a non-SARS-CoV-2 virus was detected in 54% patients (202/371) compared to only 4.1% (20/485) in 2020. SARS-CoV-2 was associated with asthma or COPD exacerbations in a smaller proportion of infected patients compared to other viruses (1.0% vs 37%).
November 23, 2020:
- SAB Comment: These two studies used data from the same database.
- Association of Body Mass Index and Age With Morbidity and Mortality in Patients Hospitalized With COVID-19: Results From the American Heart Association COVID-19 Cardiovascular Disease Registry. 11/17/20. Hendren NS. Circulation.
Obesity is an established risk factor for COVID-19 morbidity and mortality. This study quantifies and stratifies the risks along with useful tables and charts. Data from 7606 COVID-19 patients from 88 hospitals, through 7/22/20 revealed that as BMI increased, so did the relative risk of mechanical ventilation and in-hospital death. These relationships were strongest in patients <50 years, weakening with older age. BMI ≥40 was associated with an increased risk of in-hospital death only in those ≤50 years (HR 1.36). Venous thromboembolism and need for dialysis were also more frequent in the obese. Overall death rate was 17.1%. Mechanical ventilation was instituted for 21.1%. - Racial and Ethnic Differences in Presentation and Outcomes for Patients Hospitalized with COVID-19: Findings from the American Heart Association’s COVID-19 Cardiovascular Disease Registry. 11/17/20. Rodriguez F. Circulation.
As the authors note, the COVID-19 pandemic has exposed longstanding racial/ethnic inequities in health risks and outcomes in the U.S. The AHA COVID-19 CVD Registry was used. Hispanic and Black patients comprised > 1/2 of patients hospitalized with COVID-19. Though younger than non-Hispanic White patients, Hispanic and Black patients more often had lower socioeconomic status and differences in COVID-19 diagnosis and presentation characteristics. There were no differences for in-hospital mortality and major adverse cardiovascular events. Overall mortality was high, 18.4%, and Black and Hispanic patients bore a greater burden of the mortality and morbidity due to their disproportionate representation among COVID-19 hospitalizations.
- Association of Body Mass Index and Age With Morbidity and Mortality in Patients Hospitalized With COVID-19: Results From the American Heart Association COVID-19 Cardiovascular Disease Registry. 11/17/20. Hendren NS. Circulation.
- COVID-19-associated Non-Occlusive Fibrin Microthrombi in the Heart. 11/16/20. Bois MC. Circulation.
This study represents new data in autopsy results from patients with COVID-19 (n=15), influenza A/B (n=6), and non-virally mediated deaths (n=6). There were 12 COVID-19 cases with non-occlusive microthrombi and 2 cases each in the other groups. Focal myocarditis was seen in 4 active COVID-19 patients limited in extent. Direct invasion of the virus into myocardial cells was not seen. The authors conclude that the high incidence of microthrombi in the cardiac vascular system is a potential reason to use anticoagulants in these patients. A higher risk of complications including death may be seen in patients with cardiac disease, particularly those with amyloidosis. - Diaphragm Pathology in Critically Ill Patients With COVID-19 and Postmortem Findings From 3 Medical Centers. 11/16/20. Zhonghua S. JAMA Internal Med.
This research letter describes evaluation of autopsy specimens of diaphragm muscle obtained from 26 consecutive deceased COVID-19 patients, 24 of whom had been on mechanical ventilation for a mean of 12 days. Specimens from 8 deceased non-COVID-19 patients mechanically ventilated for a similar amount of time were used as a control group. ACE-2 receptors were present on diaphragm myofiber membranes in all patients. Viral RNA was found in the myofibers of 4 of the 26 COVID-19 patients. Significantly more fibrosis was present in the diaphragms of the deceased COVID-19 patients than in the diaphragms of the control patients predicting more diaphragmatic weakness in the COVID-19 patients. - Immune suppression in the early stage of COVID-19 disease. 11/18/20. Tian W. Nat Commun.
Using elegant quantitative advanced mass spectrometry proteomics and integrated data analysis with hierarchical clustering and functional correlational network strategies, these authors analyzed urine samples from COVID-19 (n=14), non-COVID-19 pneumonia cases (n=13) and healthy donors (n=10). A total of 5991 proteins were identified; 1986 proteins were significantly changed in the COVID-19 vs the other groups. More than 10 pathways significantly changed and 10x were more down-regulated than up-regulated. Showing heatmaps and protein interaction diagrams, the molecular signatures suggested a two-stage pathogenesis: immunosuppression and tight junction/cell-cell adhesion impairments early on and an activated immune response in late stages of severe COVID-19 pneumonia. - SAB Comment: Interferon (IFN) gets its name because it “interferes” with viral replication. Suspecting that interferon is inadequately produced and/or its actions blocked, two important Science papers (below) examined possible mechanisms. Zhang et al, reports finding loss of function gene variants in 3.5% of severe COVID-19 patients that control induction and amplification of Type I IFNs. The effects of these lifelong inborn variants, not found in mild disease or healthy controls, are only exposed with development of severe viral pneumonia. In the other paper, Bastard, et al, found (presumed preexisting) high-titer IgG neutralizing autoantibodies against Type I IFNs-alpha and -omega only in severe COVID-19. The autoantibodies occur in at least 2.6% of women and 12.5% of men. The defects identified by Zhang, et al, if discovered early on, could be treated with Type I IFNs, and by Bastard et al, treated with Type I IFN-beta in particular, as autoantibodies against IFN-beta are rare.
- Inborn errors of type I IFN immunity in patients with life-threatening COVID-19. 10/23/20. Zhang Q. Science.
These authors examined 659 severe COVID-19 patients for mutations in genes involved in the regulation of type I and III interferon (IFN) immunity. Following exome or genome sequencing examining rare variants at 13 candidate loci they found genetic defects in 3.5% of severe patients at eight of the 13 candidate loci involved in the TLR3- (double stranded RNA-responsive) and Interferon-regulatory factor-7 (IRF7)-dependent induction and amplification of type I IFNs. These variants resulted in enrichment of loss of function variants not found in mild COVID-19 patients or healthy individuals. Early type I IFN administration may benefit patients with these inborn variants. - Autoantibodies against type I IFNs in patients with life-threatening COVID-19. 10/23/20. Bastard P. Science.
In COVID-19 pneumonia, at least 101/987 patients had low or undetectable serum IFN-α and high-titer neutralizing IgG autoantibodies (auto-Abs) against interferon-omega (IFN-ω) (13 patients), against the 13 types of IFN-α2 (n=36), or against both (n=52). In vitro, auto-Abs blocked IFNs inhibition of SARS-CoV-2. Auto-Abs were not present in asymptomatic or mild SARS-CoV-2 infection (n=663) and in only 4/1227 healthy individuals; 95/101 with auto-Abs were men. A B cell autoimmune phenocopy of inborn errors of type I IFN immunity (seen in Zhang) accounts for life-threatening COVID-19 in at least 2.6% of women and 12.5% of men who could be treated with IFN-beta.
- Inborn errors of type I IFN immunity in patients with life-threatening COVID-19. 10/23/20. Zhang Q. Science.
- Influence of room ventilation settings on aerosol clearance and distribution. 11/16/20. Sperna Weiland NH. Br J Anaesth.
This study from the Netherlands used actual hospital rooms and ventilation systems to measure the clearance of aerosols after a simulated aerosol generating procedure. Higher air exchange rates were much more effective than manipulating the pressure gradient (i.e. negative or positive pressure rooms). A freestanding air purification unit also markedly improved aerosol removal. In positive pressure rooms, small amounts of aerosol were detected in adjacent hallways. This information could be useful when deciding on the best location for aerosol-generating procedures in SARS-CoV-2 infected patients. - Preexisting and de novo humoral immunity to SARS-CoV-2 in humans. 11/6/20. Ng K. Science.
Using diverse assays for antibodies recognizing SARS-CoV-2 proteins, these investigators examined preexisting humoral immunity to the novel and older coronaviruses in humans. Using flow cytometry, predominately IgG class cross-reacting antibodies particularly targeting the S2 subunit of the spike glycoprotein were detectable in the SARS-CoV-2-uninfected, especially children and adolescents. SARS-CoV-2 infection induced higher titers of SARS-CoV-2 S-reactive IgG antibodies, targeting both proteolytically-cleaved S1 (attachment) and S2 (entry) subunits, along with contemporaneous IgM and IgA. Notably, SARS-CoV-2-uninfected donor sera exhibited specific neutralizing activity against SARS-CoV-2 and SARS-CoV-2 S pseudotypes. Cross-reacting immunological memory may be critical to understand susceptibility to SARS-CoV-2 infection. - Safety and efficacy of inhaled nebulised interferon beta-1a (SNG001) for treatment of SARS-CoV-2 infection: a randomised, double-blind, placebo-controlled, phase 2 trial. 11/15/20. Monk PD. Lancet Respir Med.
A small company-sponsored pilot study comparing the clinical course of 48 patients treated for 14 days with a daily dose of nebulized interferon beta-1a to the clinical course of 50 placebo-treated patients as assessed by 9-point WHO Ordinal Scale for Clinical Improvement [OSCI]. Patients receiving the medication had greater odds of improvement on the OSCI scale (odds ratio 2.32) and a higher percentage of recovered patients (58% vs 35%) at the end of the observation period (day 28). The medication was well tolerated compared with placebo. Larger studies are planned. These results contrast with the absence of effect noted in a prior trial of interferon beta-1a given subcutaneously.
November 18, 2020:
- Acute Cardiovascular Manifestations in 286 Children with Multisystem Inflammatory Syndrome Associated with COVID-19 Infection in Europe. 11/9/20. Valverde I. Circulation.
A European multi-institutional study of 287 children admitted with COVID-19 demonstrated a high incidence of cardiac involvement. Most children admitted suffered GI symptoms, rash and conjunctival changes in addition to cardiac involvement. Forty percent presented with cardiac shock. Markers of cardiac involvement were present on admission including D-dimers. Treatment was not controlled. 286 were eventually discharged. Twenty-five percent had a diagnosis of coronary artery dilation by echocardiography, requiring follow-up. - Comparison of Clinical Features and Outcomes in Critically Ill Patients Hospitalized with COVID-19 versus Influenza. 11/13/20. Cobb NL. Ann Am Thorac Soc.
This is a retrospective cohort analysis “case matching” 74 seasonal influenza with 65 COVID-19 patients from 01/01/19 to 04/15/20. Diagnoses were confirmed by RT-PCR and ICU courses studied. COVID-19 patients had different demographics, longer prodrome, increased numbers of presenting symptoms and co-morbidities, higher incidence of ARDS, longer duration of mechanical ventilation and higher mortality. Includes an interesting discussion with tables. - Review of Cardiac Involvement in Multisystem Inflammatory Syndrome in Children. 11/9/20. Alsaied T. Circulation.
Though the prevalence of multisystem inflammatory syndrome in children is unknown, there have been more than 300 cases now reported in the literature. It is more common in the US in Black and Hispanic children; typically occurs a few weeks after acute infection and the putative etiology is a dysregulated inflammatory response to SARS-CoV-2 infection. Persistent fever and gastrointestinal symptoms are the most common symptoms. Cardiac manifestations are common and include ventricular dysfunction, coronary artery dilation and aneurysms, arrhythmia and conduction abnormalities, vasodilatory or cardiogenic shock requiring fluid resuscitation, inotropic support, and in the most severe cases mechanical ventilation and extracorporeal membrane oxygenation (ECMO). Most patients recover within days to a couple of weeks and mortality is rare. Long-term cardiovascular complications are not yet known. - Ventilation management and clinical outcomes in invasively ventilated patients with COVID-19 (PRoVENT-COVID): a national, multicentre, observational cohort study. 11/10/2020. Botta M. Lancet Respir Med.
This multicenter, retrospective, epidemiological study from the Netherlands examines 553 COVID-19 positive VE patients from 18 ICUs regarding the ventilatory variables (modes, TV, PEEP, *P, CTL) and its outcomes in 28 days in a comparative way.- The variations of ventilatory parameters were not different between ICUs,
- COVID-19 ARDS allows for better use of lung-protective ventilation than does ARDS due to other causes,
- All patients had low compliance,
- No conclusion for Best PEEP,
- Majority prefer to treat the refractory hypoxia by prone positioning,
- An enormous burden on ICUs/hospital systems,
- High tidal volume and low respiratory system compliance on the first day of ventilation were associated with a higher risk of 28-day mortality.
The study supports low TV, Ppl< 30, low driving pressure, prone position in ICU.
November 16, 2020:
- Analgesia and sedation in patients with ARDS. 11/10/2020. Chanques G. Intensive Care Med.
A “state of the art“ narrative review by an international panel of experts written to support clinicians in their management of ARDS patients. Proper ventilator settings, followed by analgesia, then sedation, then neuromuscular blockers form the heart of suggested approaches to analgesia and sedation. Separate sections address ARDS and COVID-ARDS, and several flow diagrams suggest various treatments. An “ABCDEF-R” approach is suggested. - Association between red blood cell distribution width and mortality of COVID-19 patients. 11/7/2020. Lorente L. Anaesth Crit Care Pain Med.
Red blood cell distribution width (RDW), a parameter of RBC form and size variability, is associated with increased mortality in a number of disease states. This prospective observational study from 8 Canary Islands ICUs analyzed data from 118 survivors and 25 deaths with COVID-19. RDW performed comparably to APACHE II and SOFA scores in predicting mortality and is easier to measure. Levels were higher on admission to ICU and when >13% predicted mortality. RBC transfusion, hemoglobin disorders, and myelodysplastic syndromes increase RDW values. - Current and evolving standards of care for patients with ARDS. 11/6/20. Menk M. Intensive Care Med.
Written by an international group of experts, this narrative review is a succinct and up-to-date review of caring for ARDS and COVID-ARDS patients, and is very useful for a frontline worker wanting a broad overview. It briefly explains the studies that establish the current standards and discusses therapies of promising interest (evolving standards). Nicely summarized in a table and discussed in the text are: ventilatory management (tidal volume, PEEP, driving pressure, mechanical power, etc.), ventilation adjuncts (proning, neuromuscular blockade, ECMO, etc.) and pharmacotherapy (steroids, fluid therapy, etc.). - Frequency of venous thromboembolism in 6513 patients with COVID-19: a retrospective study. 11/2/20. Hill JB. Blood Adv.
This single health-system venous thromboembolism (VTE) study described the use of standard heparin or LMWH prophylaxis in most of the 6513 COVID-19 patients. Dose was increased if BMI >40 and decreased if creatinine clearance < 30. Ninety-day VTE rate was 2.2% (n=86) when receiving prophylaxis vs. 11% without. Eighty-four of 86 VTE patients had received prophylaxis. PADUA Score was high in 89%. Including arterial thrombosis in 7 patients, the overall incidence of VTE was 3.1% and 7.2% if mechanically ventilated. Fifty percent inpatient VTEs met the definition of prophylaxis failure. Only three of 2075 hospitalized patients (0.14%) without VTE surviving to discharge had VTE after discharge. The authors conclude these data support a traditional approach to VTE prophylaxis both during and following hospitalization.
SAB Comment: We note a surprisingly low rate of VTE in this large, retrospective study, equally divided between DVT and PE. It did not include thrombosis in the microcirculation or ECMO circuit. Most were failures or breakthroughs on VTE prophylaxis. One may question the use of so few risk factors for modification of standard dosing and the conclusion that the data support a traditional approach. - Neutrophil extracellular traps and thrombosis in COVID-19. 11/5/20. Zuo Y. J Thromb Thrombolysis.
Forty-four patients with COVID-19 had blood collected for neutrophil extracellular traps (NETs) and neutrophil activation. Eleven of these patients developed thrombosis despite at least prophylactic heparin. Thrombosis in COVID-19 was associated with higher levels of circulating NETs and calprotectin (neutrophil activation). These data further add to the characterization of COVID-19 and the stepwise understanding of how to combat the epidemic. - Prone position in ARDS patients: why, when, how and for whom. 11/10/20. Guérin C. Intensive Care Med.
This is a thorough and excellent review of the use of prone position in ARDS including a detailed explanation of its effects on pulmonary physiology, gas exchange and hemodynamics. The significant benefits in mortality are discussed. As noted in many studies, the improvement in mortality does not correlate with the degree of oxygenation improvement but appears more likely to be related to a decrease in ventilator-induced lung injury. Specific recommendations and cautions for practical application are provided. The use of prone positioning in spontaneously breathing, non-intubated patients is commonly used with COVID-19, and studies are planned to verify if this strategy can reduce the rate of intubation and improve survival.
November 11, 2020:
- Birth and Infant Outcomes Following Laboratory-Confirmed SARS-CoV-2 Infection in Pregnancy – SET-NET, 16 Jurisdictions, March 29-October 14, 2020. 11/5/20. Woodworth KR. MMWR Morb Mortal Wkly Rep.
The authors of this article about pregnant women with SARS-CoV-2 state, “Among 3,912 infants with known gestational age born to SARS-CoV-2 infected women, 12.9% were preterm (<37 weeks), higher than a national estimate of 10.2%. Among 610 (21.3%) infants with testing results, 2.6% had positive SARS-CoV-2 results, primarily those born to women with infection at delivery.” Half of positive infants were preterm. Median maternal age was 28.9 years. Forty-six percent were Hispanic/Latina. One or more underlying medical condition was reported for 45.1%. Pre-pregnancy obesity was the most common (35.1%). Eight-four point four percent had infection identified in the third trimester. None had neonatal IgM, placental tissue or amniotic fluid testing; thus, routes of transmission could not be assessed. - Cytokine elevation in severe and critical COVID-19: a rapid systematic review, meta-analysis, and comparison with other inflammatory syndromes. 10/16/20. Leisman. Lancet.
The hypothesis that a “cytokine storm” occurring later in severe COVID-19 disease may be causative for the excess inflammatory response noted in terminal disease has provoked studies of anti-cytokine therapies, specifically interleukin-6 antagonists. This systematic review and meta analysis of studies published between November 1, 2019 and April 14, 2020, including interleukin-6 levels in the results, compared cytokine levels in four disease categories associated with elevated levels: sepsis (5,320); cytokine release syndrome (72); ARDS unrelated to COVID-19 (2,767); and COVID-19 (1,245). While COVID-19 levels were raised, the mean interleukin-6 levels in all three other conditions were statistically higher than noted in COVID (e.g. 27 times higher in sepsis and 12 times higher in non-COVID ARDS while over 1,000 times in CRS). The authors question the impact of a “cytokine storm” in COVID-19 organ dysfunction. Other arguments offered a detailed, well-presented discussion. - Cytokine Levels in Critically Ill Patients With COVID-19 and Other Conditions. 9/3/20. Kox. JAMA.
This retrospective, single-center study admitted 204 patients between 2010 and 2020 with sampling recorded plasma concentrations of proinflammatory cytokines TNF, IL-6 and IL-8 and determined (2020) in consecutively ventilated COVID-19 patients (49) with ARDS. Previously recorded levels in patients with bacterial septic shock with ARDS (51), septic shock without ARDS (15), out-of-hospital cardiac arrest (30), and multiple traumas (62) were compared with those from the COVID-19 population. COVID-19 patients had higher BMI, co-morbidities and cardiac dysfunction; however, cytokine levels were lower than in other diseases mentioned questioning the importance of a “cytokine storm” as a primary therapeutic target in COVID-19 disease.
November 9, 2020:
- Benchmarking Critical Care Well-Being: Before and After the Coronavirus Disease 2019 Pandemic. 11/2/2020. Gomez S. Crit Care Explor.
This is the result from the survey with comparison of 2 periods, 16 ICUs of 4 Hospitals to understand burnout and fulfillment among critical care healthcare (N= 482) its impact on well-being. Authors state that a rise of burnout is expanding to all across the team including APPs & Pharm D. & increased during the pandemic. These results reveal that burnout is a threat to the future of critical care team, notes that clinicians with less years of work experience were more likely to suffer adversely from burnout possibly from work load/ schedules. Professional fulfillment varied across the professional/ time/ hospital… To mitigate the burnout the Critical Care Societies Collaborative developed a “Call to Action” in 2016 & recommends that measures of well-being should be benchmarked and compared across ICUs and medical centers. Also consider offering resilience training, professional coaching, mindfulness training all across the team. - Combining lung ultrasound and Wells score for diagnosing pulmonary embolism in critically ill COVID-19 patients. 11/4/20. Zotzmann V. J Thromb Thrombolysis.
This article presents the results of a retrospective evaluation of 20 ICU COVID-19 patients who had all undergone CT pulmonary angiography and lung ultrasound for suspected pulmonary emboli in a tertiary referral ARDS/ECMO center. The study showed that subpleural consolidations ≥ 1cm detected in lung ultrasound were found frequently in COVID-19 ARDS patients with pulmonary embolism. By combining a Wells score ≥ 2 and a lung ultrasound showing subpleural consolidations, PE could be predicted with a sensitivity of 100% and a specificity of 80% in these 20 patients, 12 of whom were found to have pulmonary emboli by CT pulmonary angiography. - COVID-19 seropositivity and asymptomatic rates in healthcare workers are associated with job function and masking. 11/5/20. Sims MD. Clin Infect Dis.
This prospective cross-sectional cohort study evaluated seropositivity among 40k employees of a Detroit healthcare system who were both frontline workers and support staff, including administrators. About half of the employees participated and 8.8% were seropositive, 44% of those were asymptomatic. Those wearing N95 masks had a significantly lower seropositivity rate (10.2%) compared to surgical masks (13.1%) or no masks (17.5%). - COVID-19: what the clinician should know about post-mortem findings. 11/3/20. Jonigk D. Intensive Care Med.
This succinct and easily read editorial summarizes multisystem pathologic findings in COVID-19. Clinical presentation does not always correlate with organ involvement at autopsy. The figure illustrates alterations frequently identified in each organ system at autopsy. - Decision-making around admission to intensive care in the UK pre-COVID-19: a multicentre ethnographic study. 11/3/2020. Griffiths F. Anaesthesia.
As triage of ICU beds during COVID-19 becomes a topic of concern, this multicenter ethnographic study conducted between June 2015 and May 2016 in six UK NHS hospitals attempts to explore the decision-making process applied to ICU admissions through observations, interviews and retrospective analysis outside the pandemic. Fifty-five decision events were observed and analyzed and 44 physicians, varying in training and specialty, were interviewed. Results are reported in multiple vignettes and the heuristic nature of the decision-making process is reviewed. Suggestions for improving transparency, consistency and equity of decision‐making around ICU admission are offered. - Hematologic predictors of mortality in hospitalized patients with COVID-19: a comparative study. 10/30/20. Mousavi SA. Hematology.
This study looks over 225 COVID-19 patients in the hospital and focuses on the admission blood test as it relates to mortality. Hematologic predictors of a fatal outcome included elevated neutrophil to lymphocyte ratio and platelet lymphocyte ratio, lower than normal Hb (<12 gram/ dl) and platelet (<150,000 ), elevated D-dimer prolonged prothrombin time and elevated inflammatory indicators, higher than normal erythrocyte sedimentation rate (>15 mm/h) and C-reactive protein( > 6 mg/L). - Lack of antibodies to SARS-CoV-2 in a large cohort of previously infected persons. 11/4/20. Petersen LR. Clin Infect Dis.
In this study, sera from 2,547 known PCR+ healthcare workers and first responders were tested at least 2 weeks after symptom onset for IgG against spike protein. Sero-negativity was found in 6.3%, or 1 in 16 persons. The proportion lacking antibodies increased only slightly from 14 to 90 days post-symptom onset (p=0.06), pointing to reassurance of low sero-reversion. Sero-negativity was 0% in 79 previously hospitalized, but increased to 11.0% among 308 persons with asymptomatic infections and 31.9% on immunosuppressive medications. Black race (2.7%), severe obesity (3.9%) and those with more symptoms were less likely to be seronegative. - SARS-CoV-2 Infections Among Children in the Biospecimens from Respiratory Virus-Exposed Kids (BRAVE Kids) Study. 11/3/20. Hurst JH. Clin Infect Dis.
A BRAVE Kids study demonstrates the issues beyond the science of COVID-19 spread and infection. The sociologic impact of ethnicity (Hispanic), family life, and the role of children as a potential viral reservoir are presented. The nasopharyngeal viral loads suggest that symptom-free children might be a source for disease spread in their homes and families.
November 4, 2020:
- Characterization of Myocardial Injury in Patients With COVID-19. 10/30/20. Giustino G. J Am Coll Cardiol.
This retrospective, international, multicenter cohort study (7 hospitals in NYC and Milan) reviewed 305 patients with documented RT-PCR COVID-19 diagnosis with myocardial injury diagnosed at admission or during hospitalization. Inclusion criteria included elevated cardiac troponins, EKG abnormalities and full TTE examination. Findings indicated that severity of cardiac disease indicated by serial increases in troponins associated with graded TTE abnormalities (none, moderate, severe) was a useful prognostic indicator of outcome. Of 305 patients, myocardial injury was documented by elevated troponins in 190 (62.3%). When compared with patients with no myocardial injury, increasing severity of myocardial injury was associated with increased mortality with discrimination noted between “no” and minor TTE abnormalities versus significant abnormalities and increased inflammatory biomarkers and troponins. Effects of co-morbidities and BMI were noted as additional risk factors for myocardial damage and TTE abnormalities. - Cardiac Injury in COVID-19-Echoing Prognostication. 10/30/20. Lavie CJ. J Am Coll Cardiol.
This editorial is best summarized in the following direct quote underlining the importance of the Giustino et al manuscript. “The current recommendations of the American College of Cardiology (ACC) endorse the measurement of cTn levels when a diagnosis of acute myocardial infarction is being considered in patients with SARS-CoV-2 infection. This indication seems somehow inadequate according to the information collected by Giustino et al. (above), (12), whereby there is now evidence that Tn-positive COVID-19 patients may benefit from routine TTE, which would allow practitioners to garner useful prognostic information and to establish specific therapeutic options in patients with cardiac injury.” An excellent discussion and table are included in the editorial. - Characteristics of cardiac injury in critically ill patients with COVID-19. 10/24/20. Doyen D. Chest.
This prospective study of 43 consecutive COVID-19 positive patients admitted to two French ICUs was designed to characterize incidence and time course of cardiac injury by serial measurements of cardiac biomarkers (troponin), EKGs and echocardiographic investigations. Extensive cardiac involvement documented with 49% demonstrating injury on ICU admission and 70% experiencing injury within the 14-day observation window. New atrial dysrhythmias, and RV and LV systolic as well as diastolic dysfunction noted with greater RV systolic dysfunction associated with increased disease severity. Conclusion: Cardiac injury is common in COVID-19, occurs early in disease, and patients with injury exhibit more RV than LV systolic dysfunction.
November 2, 2020:
- SARS-CoV-2 Neutralizing Antibody LY-CoV555 in Outpatients with Covid-19. 10/28/20. Chen P. N Engl J Med.
This BLAZE-1 phase 2 interim safety analysis involved 452 mild or moderate COVID-19 outpatients within three days of diagnosis. In a study funded by Eli Lilly, patients received a single infusion of spike-protein-RBD neutralizing antibody LY-CoV555 in one of three doses (700, 2800 or 7000 mg) or placebo. Change from baseline viral load by quantitative RT-PCR at day 11 was the primary outcome and decreased in all groups. Only the middle, 2800 mg dose significantly diminished load more than placebo at day 11. All doses reduced symptoms on days 2-6, and hospitalizations (1.6% vs. 6.3%), particularly in high-risk cohorts. Although 70% had high-risk co-morbidities, no deaths occurred.
October 30, 2020:
- Aspirin Use is Associated with Decreased Mechanical Ventilation, ICU Admission, and In-Hospital Mortality in Hospitalized Patients with COVID-19. 10/23/20. Chow JH. Anesth Analg.
This multi-center cohort study of 412 COVID-19 patients explored the theory that aspirin’s anti-platelet and anti-inflammatory properties might be beneficial in lowering the risk of serious outcomes. Ninety-four patients who had taken aspirin within 7 days of admission were compared with 314 patients who had not. Aspirin use was independently associated with decreased hazard ratio (HR) of mechanical ventilation (HR 0.56), ICU admission (HR 0.57), and in-hospital mortality (HR 0.53). There were no differences in major bleeding (p=0.69) or overt thrombosis (p=0.82) between aspirin users and non-aspirin users and confounding variables were carefully controlled. Potential mechanisms are discussed including aspirin’s ability to lower interleukin-6, C-reactive protein, and macrophage stimulation. Randomized controlled trials are necessary to confirm these results. - Awake prone positioning for COVID-19 hypoxemic respiratory failure: A rapid review. 10/23/20. Weatherald J. J Crit Care.
Using a “rapid review” technique, these authors from Calgary synthesize 35 studies (none randomized) evaluating the effect of awake proning in 414 COVID-19 patients with respiratory failure. All but one study showed improvement in oxygenation while prone, but generally not sustained when returned to the supine position. 29% of patients went on to require intubation. The authors conclude that “many questions remain unanswered when considering the use of awake prone positioning.” - Convalescent plasma in the management of moderate covid-19 in adults in India: open label phase II multicentre randomized controlled trial (PLACID Trial). 10/22/20. Argwal A. BMJ.
A randomized, controlled trial of convalescent plasma (CP) in 227 treated and 224 control hospitalized patients with moderate COVID-19 from 39 hospitals in India. Patients who received 200 ml of CP x 2 had less dyspnea and fatigue and a 24% higher rate of negative PCR on day 7 (P<0.05). No difference in the levels of inflammatory markers such as ferritin, C-reactive protein, D-dimer, or LDH was observed. However, there was no difference in progression to severe disease or mortality at 28 days between groups, including a subgroup of patients who received plasma with neutralizing antibody titers >1:80. - Convalescent plasma is ineffective for covid-19. Lessons from the Placid Trial. 10/22/20. Pathak EB. BMJ.
In light of the prevalence of micro-thrombosis and the large number of thrombotic complications in COVID-19 patients, authors of this accompanying editorial highlight the pro-thrombotic properties of plasma and recommend that future blinded convalescent plasma (CP) trials exclude plasma without detectable neutralizing antibodies or treatment of control groups with other plasma. They point out that coagulation-related events in previous CP trials were not rigorously screened for their potential relationship to the treatment. - COVID-19 Gastrointestinal Manifestations Are Independent Predictors of PICU Admission in Hospitalized Pediatric Patients. 10/26/20. Gonzalez Jimenez D. Pediatr Infect Dis J.
This multicenter Spanish brief report describes 91 patients with an average age of 10. GI symptoms were the initial cause for reporting ill in 10% of children. 40% were found to have elevated LFTs. Children overall were less ill than adults; however, all 11 severely ill children suffered GI symptoms.
SAB comment: Although pediatric cases are uncommon compared to adults with multi-system illness, GI symptoms might be overlooked in children and are significant in the progress of the disease. - Improving Survival of Critical Care Patients With Coronavirus Disease 2019 in England: A National Cohort Study, March to June 2020. 10/26/20. Dennis JM. Crit Care Med.
This retrospective, observational study of COVID-19 inpatients reviewed mortality by week of admission. High dependency unit (n = 15,367) survival went from 71.6% in March/April to 92.7% in May/June while ICU (n = 5,715) went from 58% to 80.4% in the same time period. The authors attributed this to the introduction of effective treatments as part of the RECOVERY trial, improved physician understanding of the disease process, and a falling critical care burden rather than to any changes in age, sex, ethnicity or major comorbidity burden in the patient population. - Venous Thromboembolism in COVID-19. 10/25/20. Schulman S. Thromb Haemost.
This is an excellent review regarding the mechanisms and pathogenesis of the disease biomarkers and their clinical usefulness. Risk assessment models are discussed as well as the type and strength of prophylaxis based on available evidence. Recommendations or position statements from 10 sources are discussed along with treatment recommendations according to current guidelines. Thrombosis prophylaxis with low molecular weight heparin is recommended for most hospitalized patients along with a recommendation against escalating anticoagulant doses. Therapeutic anticoagulation is advised only in response to a very high suspicion or in the presence of documented venous thromboembolism. An excellent algorithm regarding VTE treatment is presented.
October 28, 2020:
- Aspergillosis Complicating Severe Coronavirus Disease. 10/21/20. Marr KA. Emerg Infect Dis.
Mounting evidence suggests that severe respiratory virus infections, especially influenza and coronavirus 2 infections, can be complicated by Aspergillus airway overgrowth with pulmonary infection characterized by mixed airway inflammation and bronchial invasion. This article reviews these issues succinctly and adds data on 20 COVID-19 patients to the growing world literature. The authors note that the syndromes of pulmonary aspergillosis complicating severe viral infections are distinct from classic invasive aspergillosis. They state that combined with severe viral infection, aspergillosis in COVID-19 pneumonia comprises a constellation of airway-invasive and angio-invasive disease and see an urgent need for strategies to improve diagnosis, prevention, and therapy.
SAB comment: An article previously highlighted in the Newsletter clarifies some of the important issues specific to diagnosing and treating pulmonary aspergillosis in COVID-19 patients. - Characteristics Associated With Racial/Ethnic Disparities in COVID-19 Outcomes in an Academic Health Care System. 10/21/20. Gu T. JAMA Netw Open.
In this cohort study of 5698 University of Michigan Health System patients tested for or diagnosed with COVID-19, preexisting type 2 diabetes or kidney diseases and living in high–population density areas were associated with higher risk for COVID-19 hospitalization. Adjusting for covariates, non-Hispanic Black patients were 1.72-fold more likely to be hospitalized than non-Hispanic White patients, though the reasons for hospitalization were not defined. However, no significant race differences were observed in intensive care unit admission and mortality. - Reusability of filtering facepiece respirators after decontamination through drying and germicidal UV irradiation. 10/22/2020. Vernez D. BMJ Glob Health.
A “drying cycle” (30 min, 70°C) plus 60 mJ/cm2 of UV-C irradiation (UVGI) effectively decontaminated 2 Staphylococcus aureus’ bacteriophages on 2 models of FFP2 disposable respirators (the European standard most similar to N95) with preserved functional characteristics after 10 cycles. (n=12) Testing included cultures, scanning electron microscopy, Fourier-transform infrared spectroscopy, 10–300 nm NaCl aerosol particle penetration, and visual inspection. 4 respirators treated with the heat alone showed complete decontamination of the phages however UVGI adds protection. H2O2 production during UVGI was observed. Respirators worn for 1 work shift showed slightly increased particle penetration. No fit testing reported. - What have we learned ventilating COVID 19 patients? 10/12/20. Trahtemberg U. Intensive Care Med.
These leaders in ARDS research provide a crisp review of ventilatory management of COVID-19-induced ARDS (CARDS), based on the underlying pathophysiology and contend that the similarities in the spectrum of CARDS versus that of non-COVID ARDS outweigh the differences. They find a paucity of data exists to justify early intubation. They favor lung protective ventilation for all patients, and they argue for prone positioning for patients with moderate-to-severe ARDS (PaO2/FiO2 ratio < 150 mmHg). In summary they write, “ventilatory management of patients with COVID-19 ARDS should be similar to that for other causes of ARDS, tailored to the specific patient.”
October 26, 2020:
- Efficacy of Tocilizumab in Patients Hospitalized with Covid-19. 10/21/20. Stone JH. N Engl J Med.
This is a prospective, randomized, placebo-controlled study where treated patients received a single dose of 8mg/kg of tocilizumab (161 of 243 enrolled patients). The results showed that tocilizumab was not effective for preventing intubation or death in moderately ill hospitalized patients with COVID-19. - Physiological and quantitative CT-scan characterization of COVID-19 and typical ARDS: a matched cohort study. 10/21/20. Chiumello D. Intensive Care Med.
This detailed Italian physiologic study compared 32 COVID-19 ARDS (CARDS) patients with two other matched historical groups of typical ARDS patients; one matched with the CARDS patients by SpO2/FiO2, and one matched by respiratory compliance. As noted previously by this group (but not some studies by other groups), they found CARDS patients to have higher compliance than the group of non-COVID ARDS patients who were matched for SpO2/FiO2. They also found the CARDS patients had lower SpO2/FiO2 than non-COVID ARDS patients who were matched for compliance. Increasing PEEP from 5 to 15 improved oxygenation in CARDS patients but did not improve respiratory mechanics or CO2 clearance as usually seen in ARDS. These authors continue to recommend low PEEP and low driving pressure in early CARDS. - Prediction models for covid-19 outcomes. 10/21/2020. Sperrin M. BMJ.
A risk prediction algorithm to estimate hospital admission (n=10,776) and mortality (n=4,384) from covid-19 was created and validated using a UK dataset derived from 6.08 million 19-100 year old patients and validated with data from an additional 2.17 million. Study period was Jan 24-April 30 for the initial cohort and May 1-June 30, 2020 for the validation cohort. The model, including age, ethnicity, deprivation, BMI, and a range of comorbidities, predicted ¾ of deaths with excellent discrimination (Harrell’s C statistics >0.9). People in the top 20% of predicted risk of death accounted for 94% of deaths. - Living risk prediction algorithm (QCOVID) for risk of hospital admission and mortality from coronavirus 19 in adults: national derivation and validation cohort study. 10/21/2020. Clift AK. BMJ.
Editorial discussing the potential utility of prediction models referencing article 1528 and a second BMJ report published in September on the 4C mortality score (calculated at hospital admission to predict in-hospital mortality for patients with confirmed or likely covid-19). Models have serious shortcomings and require constant updating however may also inform public health policies, vaccine allocation, and provide decision support for treatment. - Sensible Medicine—Balancing Intervention and Inaction during the COVID-19 Pandemic. 10/15/20. Seymour CW. JAMA.
This article, which contains a discussion relevant for all practitioners engaged in clinical care cautions against abandoning clinical experience and consultation for early adoption of unproven and potentially harmful therapies. The authors urge that practitioners use sensible medicine, a blend between doing nothing and going all in. Their argument is well illustrated and supports the current therapeutic state in which good clinical care in well-managed ICUs following established protocols appears to be effective management strategy. No therapeutic agent has demonstrated significant mortality benefit with the exception of dexamethasone administered appropriately. The discussion supports the decision to steer a middle course with elegance and logic and is refreshing, timely and relevant. - Targeting complement cascade: an alternative strategy for COVID-19. 10/19/20. Ram Kumar Pandian S. 3 Biotech.
The authors present well-referenced experimental support that complement cascade inhibition will counteract COVID-19 inflammation. Complement dysregulation can lead to cytokine storm and ARDS pathology. Activation and deposits of complement components are seen in animal models and at autopsy of COVID-19 patients. Pre-clinical and clinical studies using current and pipeline agents show pathway inhibition aids ARDS recovery. Viral infections including COVID activate complement via the lectin pathway via mannose-binding lectin associated serine protease 2 (MASP2). Complement inhibitors including monoclonal antibodies, proteins, peptides and small molecules exhibit promise blocking the complement components and their downstream effects in various pathological conditions including SARS-CoV. - Time to Reassess Tocilizumab’s Role in COVID-19 Pneumonia. 10/20/20. Parr JB. JAMA Intern Med.
The author’s conclusions in this excellent editorial are informed by three studies (two are randomized prospective) reported in this issue of JAMA Internal Medicine and by two additional randomized prospective studies. Although observational studies by the STOP-COVID investigators and others report mortality benefit and other positive outcomes, findings from the randomized prospective trials described herein (total of 542 patients treated) do not support routine tocilizumab use in COVID-19. A well-constructed summary table of the five studies is provided.
October 23, 2020:
- Coagulopathy, endothelial dysfunction, thrombotic microangiopathy and complement activation: potential role of complement system inhibition in COVID-19. 10/16/20. Wang X. J Thromb Thrombolysis.
This article reviews the data for the role of the complement system in COVID-19. It reviews the prior (limited) data in humans to control the complement system. - COVID-19-Associated Coagulopathy and Inflammatory Response: What Do We Know Already and What Are the Knowledge Gaps? 10/20/20. Görlinger K. Anaesth Analg.
This is a comprehensive review of many aspects of COVID-19 and coagulopathy. The article identifies questions that still need to be explored. The essence of each study is summarized succinctly and its clinical impact highlighted. - COVID-19 Coagulopathy and Inflammation: The Knowns and Unknowns. 10/20/20. Wanderer JP. Anesth Analg.
This infographic, which accompanies the article by Görlinger, is useful and again raises areas that need to be explored.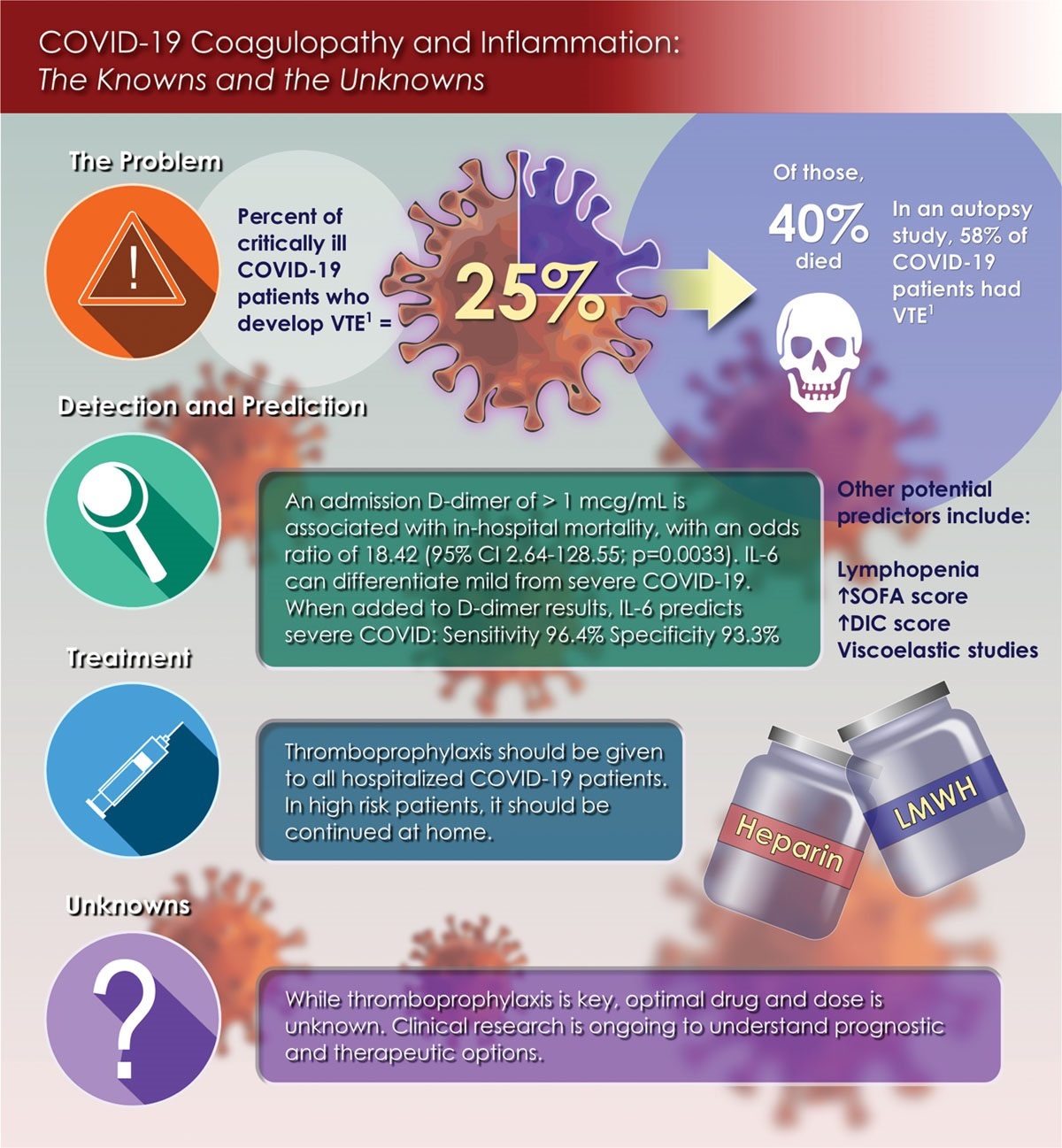
- Pasteurization Inactivates SARS-CoV-2 Spiked Breast Milk. 10/22/20. Conzelmann C. Pediatrics.
Bench Research, Human Milk, and SARS-CoV-2. 10/22/20. Furman L. Pediatrics.
A team of German virologists determined that the SARS-CoV-2 virus can be shed and is detectable in human breast milk but does not replicate in that environment. Inoculation of breast milk with various strains of the virus resulted in a 40-90% decrease in viral titer due to antiviral properties of breast milk alone. Heating to 63°C (145°F) for 30 minutes (Holder pasteurization) completely inactivated the virus.
Welcoming these findings, an accompanying editorial by two US pediatricians is strongly in favor of allowing infected mothers to breastfeed their babies whenever possible as the milk duct epithelium’s lack of proteases required to allow virus entry prevents vertical transmission of COVID-19 from an infected mother. - Rotational thromboelastometry results are associated with care level in COVID-19. 10/17/20. Almskog LM. J Thromb Thrombolysis.
Rotational thromboelastometry (ROTEM) is a method to identify hypercoagulability based on viscoelastic measurements of clot formation and firmness. Authors of this Swedish prospective, observational, single-center study evaluated the ability of ROTEM to estimate disease severity in 60 adult COVID-19 ward and ICU patients. Compared to 86 healthy controls, values showed increased coagulability in patients with mild disease and marked increases in those with severe disease. The ROTEM changes showing hypercoagulability occurred earlier than elevations in D-dimer. Authors concluded these preliminary data justify larger randomized trials.
From the SAB: ROTEM is a proprietary variety of thromboelastometry. Principles of this study may apply to other measurement techniques, including thromboelastography (TEG).
October 21, 2020:
- Famotidine Use Is Not Associated With 30-day Mortality: A Coarsened Exact Match Study in 7158 Hospitalized COVID-19 Patients from a Large Healthcare System. 10/15/20. Yeramaneni S. Gastroenterology.
This large retrospective study from HCA Healthcare repudiates 2 smaller studies from Columbia and Hartford which reported a two-fold reduction in risk of death or intubation for COVID-19 inpatients. One thousand one hundred twenty-seven patients (15.7%) received famotidine and 6031 (84.3%) did not. Applying multivariable logistic regression within a carefully matched cohort showed no association between in-hospital famotidine use and 30-day mortality after adjustment for WHO severity, smoking status, and listed medications.
SAB Comment: Due to famotidine’s ability to inhibit a protease essential for SARS-CoV-2 virus replication in vitro, it is under intense study in many centers. A clinical trial administering high-dose IV treatment (120 mg IV q8h) is currently under way at Columbia. - The duration of infectiousness of individuals infected with SARS-CoV-2. 10/13/20. Walsh KA. J Infect.
The potential duration of patient infectiousness, as derived from virus culture and contact tracing studies, for those individuals in whom SARS-CoV-2 RNA is detected is summarized. Thirteen various quality studies and 2 large contact tracing studies were included. The data suggests that COVID-19 patients with mild-to-moderate illness are highly unlikely to be infectious beyond 10 days from symptom onset. Evidence from a limited number of studies indicates that patients with severe-to-critical illness, and/or those who are immunocompromised, may be infectious for a prolonged period, possibly for 20 days or more. Research is needed to confirm these findings and to provide information on the duration of infectiousness in subgroups such as children, and asymptomatic and immunosuppressed patients. - Transmission Dynamics by Age Group in COVID-19 Hotspot Counties – United States, April-September 2020. 10/15/20. Oster AM. MMWR Morb Mortal Wkly Rep.
CDC analyzed temporal trends in percent test positivity by age group in COVID-19 hotspot counties before and after their identification as hotspots. Among 767 U.S. hotspot counties identified during June and July 2020 (24% of counties, 63% of population) early increases in the percent positivity among persons 24 years old and younger were followed by several weeks of increasing percent positivity in persons 25 years old and older, particularly those in the South and West. Addressing transmission among young adults is an urgent public health priority.
October 19, 2020:
- A score combining early detection of cytokines accurately predicts COVID-19 severity and intensive care unit transfer. 10/2/2020. Nagant C. Int J Infect Dis.
These investigators prospectively examined (n=63) levels of twelve serum cytokines following admission (days 0-3) to seek combinations that could discriminate progression to severe (PaO2 <93% or PaO2/FiO2≤300 mmHg) vs non-severe disease and predict ICU transfer (ventilator/ICU monitoring). Combinatorial (multiplication of levels of IL-6, IL-10, IL-8) score had the highest sensitivity and specificity to predict severe disease (n=44) at a cutoff value of 2068 pg/mL vs non-severe disease (n=19). Levels of IL-6 x IL-10 (cut-off value of 178 pg/mL) predicted ICU transfer (n=35) vs non-critically ill (n=28). Use of this score could improve patient triage and therapeutic strategies within clinical trials. - Acute Respiratory Distress Syndrome: Contemporary Management and Novel Approaches during COVID-19. 10/5/20. Williams GW. Anesthesiology.
This is a succinct, well-written review of best practice treatment strategies for non-COVID-19 ARDS with research-based updates on appropriate strategies for COVID-19 associated-ARDS treatments. Figures and brief descriptions are provided on the research supporting low tidal volumes, PEEP levels, prone positioning, PaO2 targets, steroid treatment, fluid management, ECMO and early neuromuscular blockade. - Aerosolisation during tracheal intubation and extubation in an operating theatre setting. 10/12/20. Dhillon RS. Anaesthesia.
This study reports measurements and size characterization of aerosols generated and spread throughout a standard positive pressure operating room (with 26 room volume air exchanges per hour) during intubation and extubation of 3 study patients. Face-mask ventilation, tracheal tube insertion and cuff inflation generated small particles 30–300 times above background noise that remained suspended in airflows and spread from the patient’s facial region throughout the confines of the operating room. The authors believe that these findings support careful use of PPE throughout standard ventilation operating rooms. - Blood purification therapy with a hemodiafilter featuring enhanced adsorptive properties for cytokine removal in patients presenting COVID-19: a pilot study. 10/12/2020. Villa G. Crit Care.
Italian preliminarily prospective observational study of 37 patients receiving immunomodulatin or support of renal function using Baxter’s oXiris heparin-coated extracorporeal hemodiafilter Feb-April 2020. Compared to the expected (65%!) mortality rates, as calculated by APACHE IV, the mean observed rates were 8.3% lower after treatment. Reduction in serum IL-6 concentrations correlated with improved organ function, measured as decreased SOFA score. The best improvement in mortality rate was observed in patients receiving early treatment during in ICU. Anticoagulation regimens were inconsistent. 7 treatments (19%) resulted in clotting. - Convalescent plasma for patients with severe COVID-19: a matched cohort study. 10/10/20. Rogers R. Clin Infect Dis.
This small study from 3 hospitals compared 64 recipients of 1-2 units of CP (median 7 days after symptom onset) with 177 matched controls. Neither in-hospital mortality (~15%) nor overall rate of hospital discharge differed significantly, although the rate of hospital discharge among patients older than 65 years who received convalescent plasma (CP) was significantly higher (RR 1.86, 95% CI 1.03 – 3.36). There was a greater than expected frequency of transfusion reactions in the CP group (2.8% per unit transfused). Authors suggest adequately powered randomized studies should target patients older than 65 years when assessing CP treatment efficacy. - COVID-19 Transmission in US Child Care Programs. 10/1/20. Gilliam WS. Pediatrics.
This is an analysis of a survey completed in late May 2020 by 57,335 childcare providers from all 50 states that were asked about their exposure, their transmission mitigation efforts and whether or not they had ever tested positive for having COVID-19. While 427 (0.7%) of the respondents had tested positive, there was no association found between exposure to childcare and contracting COVID-19. The authors note that results may depend upon the mitigation efforts taken (outlined in the article) and on the relatively low prevalence rates across the United States at the time of the study. Transmission home to parents or siblings was not evaluated. - Evidence of a wide gap between COVID-19 in humans and animal models: a systematic review. 10/7/2020. Ehaideb SN. Crit Care.
In this comprehensive literature review, replication-competent animal models were assessed for recapitulating full-spectrum human COVID-19, as well as prophylaxis, therapies, or vaccines. Animals included nonhuman primates (n = 13), mice (n = 7), ferrets (n = 4), hamsters (n = 4), and cats (n = 1). All animals supported high viral replication in the respiratory tract with mild clinical manifestations, lung pathology, IgG antibodies and full recovery. Older animals had more severe illness. None developed respiratory failure, multiple organ dysfunction or death. Transient systemic inflammation was observed occasionally in nonhuman primates, hamsters, and mice. No animals unveiled cytokine storms or coagulopathy supporting a wide gap between human and animal disease. - Longitudinal Profile of Laboratory Parameters and Their Application in the Prediction for Fatal Outcome Among Patients Infected With SARS-CoV-2: A Retrospective Cohort Study. 10/13/2020. Zeng HL. Clin Infect Dis.
In this retrospective study of 642 patients with COVID-19, 55 laboratory values profiled along the entire disease course. Three distinct clinical stages were identified: a. acute stage 1-9 days after symptoms, slightly deviated indicators of liver damage, renal damage, and impaired immunity; b. the second stage, 10–15 days after disease onset, with corresponding ICU admission, and c. a third or convalescence stage with clinical symptoms beginning to resolve and laboratory measurements gradually reverting to normal, compared to thrombocytopenia and decreases in monocytes, exclusively observed in fatal cases; LDH, PCT, lymphocyte count, and IL-6 t were highly important prognostic markers. - The Effect of Temperature on Persistence of SARS-CoV-2 on Common Surfaces. 10/7/20. Riddel S. Virology.
In this study, SARS-CoV-2 viability was measured on polymer and paper bank notes, stainless steel, glass, vinyl and cotton cloth at 20, 30, and 40°C. High titer virus was applied, and samples stored in the dark at 50% relative humidity. Half-lives were a few days on all surfaces at 20°C and reduced to a few hours at 40°C. Hard surfaces support viable virus longer than absorbent ones. Some remained detectable for 28 days on nonabsorbent surfaces at ambient temperature. Fomite transmission may be more important than previously thought. Concerns regarding bank notes, touchscreens and mobile phones are of particular importance. - The Impact of High-Flow Nasal Cannula Use on Patient Mortality and the Availability of Mechanical Ventilators in COVID-19. 10/13/2020. Gershengorn HB. Ann Am Thorac Soc.
This sophisticated simulation looked at scenarios of COVID-19 surges in the US as a whole, with variable strategies for using high flow nasal oxygen (HFNO) and invasive mechanical ventilation (IMV). The strategy that resulted in the fewest deaths and greatest ventilator availability was using HFNO initially, coupled with early IMV when ventilator supply was sufficient. - The impact of protocol-based high-intensity pharmacological thromboprophylaxis on thrombotic events in critically ill COVID-19 patients. 10/12/20. Atallah B. Anaesthesia.
This study was conducted to discover if high-intensity thromboprophylaxis would lead to fewer thrombotic events in COVID-19 positive patients. These patients were selected for high-intensity thromboprophylaxis when the D-dimer level was > 2ug/ml, and for therapeutic anticoagulation when the level was >3ug/ml. High-intensity thromboprophylaxis (enoxaparin 40 milligrams bid), but not therapeutic anticoagulation was associated with fewer thromboembolic events. Low D-dimer levels were independently associated with fewer venous thromboembolism events. Bleeding events in the high intensity thromboprophylaxis group were 2.7% compared to 16.5% using therapeutic anticoagulation. The authors conclude that high intensity thromboprophylaxis may reduce the incidence of thrombotic events without a significant increase in bleeding. - Treatments Considered for COVID-19. 10/15/20. The Medical Letter.
This latest edition of The Medical Letter’s “Treatments Considered for COVID-19” was released on October 15, 2020 and included comprehensive (over 100 pages) up-to-date tables of drug, vaccine and other treatment classes. The columns include “Drug and Dosage,” “Efficacy,” “Adverse Effects/Interactions” and “Comments,” all with thorough referencing.
Updates added to this edition include:- remdesivir – new guidelines from NIH and IDSA,
- convalescent plasma – new guidelines from IDSA,
- monoclonal antibodies, mesenchymal stem cell therapy, corticosteroids – new guidelines from NIH and IDSA,
- IL-6 Inhibitors – new guidelines from IDSA; JAK inhibitors – data from NIH’s ACTT-2 trial on baricitinib, and
- antimalarials – results from the RECOVERY trial, PPIs, vaccines and SSRIs.
October 14, 2020:
- A quantitative evaluation of aerosol generation during tracheal intubation and extubation. 10/6/20. Brown J. Anaesthesia.
This is a pertinent report on measurement of 0.3-10 nm aerosolized particles using real-time, high-resolution environmental monitoring in ultraclean ORs with laminar flow ventilation and 500–650 air changes / hour. Tracheal intubation sequences including face-mask ventilation produced very low particle quantities (average concentration, 1.4 particles/L, n = 14, p < 0·0001 vs. cough). Tracheal extubation, particularly when the patient coughed, produced a detectable aerosol (21 particles/L, n = 10), 15-fold greater than intubation (p = 0.0004) but 35-fold less than a volitional cough (p < 0.0001). The study does not support the designation of elective tracheal intubation as an aerosol-generating procedure. - Duration of Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) Infectivity: When Is It Safe to Discontinue Isolation? 10/8/20. Rhee C. Clin Infect Dis.
In the review, SARS-CoV-2 is most contagious right before and immediately after symptom onset, and contagiousness rapidly decreases to near-zero about 10 days from symptom onset in mild-moderately ill patients and 15 days in critically ill and immunocompromised patients. The longest duration of viral viability reported is 20 days from symptom onset. Persistently positive SARS-CoV-2 RNA PCR does not indicate replication-competent virus and is not associated with contagiousness. Chain reaction assays that alternate between positive and negative results in recovered patients from COVID-19 most likely reflect sampling variability. The infection confers at least short-term immunity in most cases, but duration of immunity is unclear and several cases of re-infection have now been confirmed. - In-hospital cardiac arrest in critically ill patients with covid-19: multicenter cohort study. 9/30/20. Hayek S. BMJ.
This article discusses a multicenter (68 sites) US study which followed 5019 admitted COVID-19 patients, 701 (14%) of whom had in-hospital cardiac arrest. The influence of patient demographics, co-morbidities and critical care facilities on outcome are also described. Patients younger than 45 years were more likely to receive CPR with 21.2% (11/52) surviving to hospital discharge with normal or mild neurocognitive deficit compared to 2.9% in patients 80 years or older. The article confirms generally poor results of CPR in COVID-19 but provides interesting discrimination between age, ICU size and co-morbidities. It raises key questions regarding triage and informed assent discussions. - Lopinavir-ritonavir in patients admitted to hospital with COVID-19 (RECOVERY): a randomised, controlled, open-label, platform trial. 10/5/20. RECOVERY Collaborative Group. Lancet.
This article reports results of a prospective, controlled, open-label adaptive platform trial designed to test effectiveness of lopinavir-ritonavir (1616) against usual care (3424) in patients admitted to hospital with COVID-19 between March 19 and June 29. Lopinavir-ritonavir treatment was not associated with any primary endpoint benefit, including 28-day mortality, hospital length of stay, risk of progressing to mechanical ventilation or death. The results do not support use of lopinavir-ritonavir to treat COVID-19 patients. - Antiviral monotherapy for hospitalised patients with COVID-19 is not enough. 10/5/20. Cao B. Lancet.
Commentary on accompanying article findings from the RECOVERY trial that lopinavir-ritonavir addition to usual care in managing COVID-19 patients admitted to hospital conveyed no outcome benefit for the primary endpoints of death at 28 days, hospital length of stay or progression to mechanical ventilation. The authors suggest that despite negative trial results, future research in this area should continue and that evaluation and efficacy of antiviral and immunomodulator combination therapy be continued.
October 12, 2020:
- Clinical criteria for COVID-19-associated hyperinflammatory syndrome: a cohort study. 9/29/20. Webb BJ. Lancet Rheumatol.
Defining the scourge of COVID-19 hyperinflammatory syndrome. 9/29/20. Cron RQ. Lancet Rheumatol.
These authors are first to propose specific criteria for COVID-19-associated hyperinflammatory (cytokine storm) syndrome (cHIS). They validated the cHIS scale using retrospective data from 299 COVID-19 inpatients from their 22-hospital system. The six-criterion additive scale: fever, macrophage activation (hyperferritinemia), hematological dysfunction (neutrophil to lymphocyte ≥10:1 ratio), hepatic injury (lactate dehydrogenase or aspartate aminotransferase), coagulopathy (D-dimer), and cytokinemia (C-reactive protein, interleukin-6, or triglycerides). Meeting ≥2 criteria was associated with increased mortality and mechanical ventilation risk. External validation is needed. The cHIS scale may better target populations for trials and immunomodulation and diminish heterogeneity of treatment effect analyses of trials with undifferentiated patients. - Compassionate Use of Remdesivir in Pregnant Women with Severe Covid-19. 10/8/20. Burwick RM. Clin Infect Dis.
This is a multicenter review of the outcomes for 67 pregnant and 19 immediate post-partum patients with moderate to severe COVID-19 treated with remdesivir. Outcomes were generally good, but there was no comparison to a control group. Remdesivir was well tolerated, with a low incidence of serious adverse events (16%). Most adverse events were related to pregnancy and underlying disease; most laboratory abnormalities were Grades 1 or 2. There was one maternal death attributed to COVID-19 and no neonatal deaths. - Remdesivir for Adults With COVID-19: A Living Systematic Review for an American College of Physicians Practice Points. 10/5/20. Wilt TJ. Ann Intern Med.
Of the 89 pertinent articles that these authors reviewed, only 4 fit their strict criteria and were chosen for this review. They concluded that from the best evidence available so far, remdesivir probably improves recovery, reduces serious adverse events and may reduce mortality and time to clinical improvement in hospitalized adults with COVID-19. For patients not on a ventilator, a 5-day course may provide similar benefits to, and fewer harmful effects, than a 10-day course. The review is titled “Living” because these authors, from the VA system, plan to update their literature search every 2 months through December 2021. - Remdesivir for the Treatment of Covid-19 — Final Report. 10/8/20. Beigel JH. N Engl J Med.
This article is a follow-up to the initial “preliminary report” that was published May 22, 2020 and was included as 47% of the patients in the review above. This “final report” of the ACTT-1 study provides later outcomes and analysis of the same 1062 patients in the “preliminary” report, randomized between February 21 and April 19 to receive 10 days of remdesivir or placebo. Similar to the analysis in the first report, those who received remdesivir had a median recovery time of 10 days compared with 15 days among those who received placebo. Kaplan–Meier estimates of mortality were 6.7% with remdesivir and 11.9% with placebo by day 15 and estimates of mortality by day 29 (new in this report) were 11.4% with remdesivir and 15.2% with placebo. - Susceptibility of tree shrew to SARS-CoV-2 infection. 9/29/2020. Zhao Y. Sci Rep.
SARS-Co-V-2 research has been hampered by poor susceptibility of animal models to SARS‑CoV‑2 infection, particularly the mouse. These investigators examined if a domesticated tree shrew, a species genetically close to primates and used in hepatitis, influenza and other research may be useful. SARS-CoV-2-infected tree shrews showed no clinical signs except mild fevers. Histologically, low levels of virus shedding and replication in tissues were observed. Mild pulmonary abnormalities were the main changes observed. The tree shrew may not be suitable for COVID‑19 research. However, tree shrew may be a potential asymptomatic intermediate host of SARS‑CoV‑2 besides bats and pangolins. - Updated guidance on the management of COVID-19: from an American Thoracic Society/European Respiratory Society coordinated International Task Force (29 July 2020). 10/6/20. Bai C. Eur Respir Rev.
In this article, the Task Force (American Thoracic Society/European Respiratory Society coordinated International Task Force 29 July 2020) make consensus suggestions to treat patients with acute COVID-19 pneumonia with remdesivir and dexamethasone but not with hydroxychloroquine except in the context of a clinical trial. COVID-19 patients with a venous thromboembolic event can be treated with therapeutic anticoagulant therapy for 3 months. Routine screening of patients for depression, anxiety and post-traumatic stress disorder was also suggested by the task force.
October 9, 2020:
- Psychological Impact of COVID-19 on ICU Caregivers. 9/29/20. Caillet A. Anaesth Crit Care Pain Med.
In this survey conducted among 208 ICU staff of a French teaching hospital, the incidence of anxiety and depression was 48% and 16% respectively, and PTSD was present in 27%. Use of the “Hospital Anxiety and Depression Scale” (HADS) and “Impact of Event Scale – Revised” (IES-R) revealed lack of critical care training as an important independent risk factor for anxiety syndrome and PTSD. COVID-19 unit assignment was responsible for anxiety syndrome and a prior history of burnout were risk factors for PTSD. The authors suggest intensified training and awareness of individuals’ history to address some of these issues. - Surgical mask on top of high-flow nasal cannula improves oxygenation in critically ill COVID-19 patients with hypoxemic respiratory failure. 9/29/20. Montiel V. Ann Intensive Care.
This study (n= 21) points out that placing a surgical mask on a patient’s face along with high-flow nasal cannula (heated / humidified/ 60 L/m device), had a statistically significant improvement of oxygenation (PaO₂:FiO₂, saturation, PaO₂) in COVID-19 hypoxemic respiratory failure. They noted an insignificant change in PaCO₂. This suggests the usefulness of a small change of a modality which can be rendered safely outside the ICUs in an overwhelming surge. Authors advocate that this step precede non-invasive ventilation to improve oxygenation. - Survival of SARS-CoV-2 and influenza virus on the human skin: Importance of hand hygiene in COVID-19. 10/3/20. Hirose R. Clin Infect Dis.
In this in vitro cadaveric skin model, and insert surfaces, these investigators noted that COVID viruses survive statistically significantly longer (8x) when compared with influenza virus. The authors found the virus can be completely inactivated within 15 seconds of exposure to 80% (w/w) ethanol. Thus, appropriate hand hygiene using ethanol-based disinfectants leads to rapid viral inactivation and may reduce the risk of contact infections. It should be noted that these studies were carried out at room temperature, which may allow longer viral viability compared with normal in vivo skin temperature. - Therapeutic versus prophylactic anticoagulation for severe COVID-19: A randomized phase II clinical trial (HESACOVID). 9/20/2020. Lemos ACB. Thromb Res.
This paper randomized 20 COVID-19 patients requiring mechanical ventilation. Ten patients were assigned to either therapeutic enoxaparin (enoxaparin) or to prophylactic anticoagulation (SQ heparin). There was an increase in the PaO2/FiO2 ratio in the therapeutic group, p=0.0004 which was not seen in the prophylactic group, p=0.487. Patients in the therapeutic group had a rate of successful liberation from mechanical ventilation (hazard ratio: 4.0, p=0.031) and more ventilator-free days (15 days versus 0 days, p = 0.028). There was no difference in mortality. While the dataset is small, it does show promise and is an introduction for larger upcoming trials.
October 7, 2020:
- Clinical Outcomes of In-Hospital Cardiac Arrest in COVID-19. 9/28/20. Thapa S. JAMA Int Med.
This research letter reports single-center results of CPR in 60 COVID-19 patients out of 1309 admitted between March 15 and April 3 who developed cardiac arrest (4.6%). Non-shockable rhythms presented in 52 (96.3%) with no patients surviving to discharge. The discussion notes results of CPR with those previously reported for in-hospital cardiac arrest (25% with 86% presenting non-shockable) and provides potential consequences of COVID-19. The authors suggest the importance of further research and consideration of guidelines for CPR in COVID-19. - Outcomes of Cardiopulmonary Resuscitation in Patients With COVID-19—Limited Data but Further Reason for Action. 9/28/20. Modes M. JAMA Int Med.
Important discussion based on dismal post-CPR outcomes in accompanying research letter. While recognizing the difficulties of performing CPR in COVID-19 patients, the importance of developing a clearly defined care plan following a detailed, continuing discussion on outcome prognosis between the healthcare team and patient-family unit is emphasized. The concept of initiating an informed assent with the family in which the care team makes real-time decisions on DNAR (do not attempt resuscitation) is raised. Additionally, healthcare disparities and associated availability of advanced care directives highlight need for healthcare systems to adopt clearly defined protocols and emphasizes “goals of care” discussion between patients and families. Resource links provided. - Epidemiology and transmission dynamics of COVID-19 in two Indian states. 9/30/20. Laxminarayan R. Science.
A data-rich epidemiologic study from 2 states in India, demonstrating the spread of COVID-19. Mortality increased with age. Underlying conditions which increased mortality included male sex, and in older patients included hypertension, obesity, and diabetes. Younger patients who died suffered underlying conditions of the liver and kidneys. - Glucocorticoid therapy does not delay viral clearance in COVID-19 patients. 9/21/20. Ji J. Crit Care.
In this letter, the authors report retrospectively on viral clearance in mild and severe cases of COVID-19, including those receiving steroids. Viral clearance ranged between 11 and 52 days. Viral clearance was defined as having three continuously negative RT-PCR tests. There was no difference in the cohort receiving steroids. - Immune responses to SARS-CoV-2 infection in hospitalized pediatric and adult patients. 9/21/20. Pierce CA. Science Translational Medicine.
A small but complex study from New York of 90 patients total, split into two groups of younger than 24 years and older than 24 years. The study demonstrated clear differences in the immune response with a robust response of IL-17A in the younger age which had fewer deaths and a greater T cell response in older patients whose health was more complicated and for whom death was more common. Treatment and medications were not controlled between the groups. Of note, the angiotensin-renin system was not studied. - Portable pocket-sized ultrasound scanner for the evaluation of lung involvement in COVID-19 patients. 9/21/20. Bennett D. Ultrasound in Medicine & Biology.
No significant differences were found between lung ultrasound scores obtained with a high-end or a portable pocket-sized ultrasound scanner on 437 paired readings in 34 LUS evaluations of hospitalized patients, including patients with mild (n=7), moderate (n=11) and severe (n=16) disease. The tested pocket-sized scanner has a single silicon chip containing a 2D array of 9000 capacitive micromachined ultrasound transducers instead of the standard piezoelectric crystal-based transducers. The chip emulates curved, linear, or phased transducers in M-mode, B-mode or color Doppler with a 2–30 cm scan depth. - Safety and 30-day outcomes of tracheostomy for COVID-19: a prospective observational cohort study. 9/29/2020. Queen Elizabeth Hospital Birmingham COVID-19 airway team. Br J Anaesth.
This prospective, non-randomized study from the UK evaluated 164 mechanically ventilated patients, 100 of whom received tracheostomy by a trained team. Despite similar characteristics and APACHE II scores, 30-day survival was higher after tracheostomy (85%) compared with no tracheostomy (42%), and ICU stay was shorter. None of the airway team involved contracted COVID-19. Contrary to earlier guidelines recommending limited or late tracheostomy, this study suggests that early tracheostomy is safe and has benefits. - The US Strategic National Stockpile (SNS) Ventilators in COVID-19: A Comparison of Functionality and Analysis regarding the Emergency Purchase of 200,000 devices. 9/14/20. Branson R. Chest.
Recognized disaster experts reviewed the capabilities of the ventilators available in the Strategic National Stockpile (SNS) before COVID-19, and those ordered by the US government under an Emergency Use Authorization. About half of these are not designed to support the sickest COVID-19 patients, and many have important limitations, such as lack of pediatric capability, lack of flow-volume loops, missing parts, difficult user learning curves, lack of maintenance availability, etc. Each of the currently available ventilators in the SNS is described, and suggestions for updates to the ventilator SNS stockpiles are made.
October 5, 2020:
- Convalescent Plasma for the Treatment of COVID-19: Perspectives of the National Institutes of Health COVID-19 Treatment Guidelines Panel. 9/25/20. Pau AK. Ann Intern Med.
Data are currently insufficient for the NIH to recommend for or against convalescent plasma (CP) for COVID-19. Enrollment in adequately powered US RCTs is slow.FDA analysis (4330 patients):
- 7-day mortality following high-titer vs. low-titer plasma
- No difference overall.
- Intubated patients (~1/3) – No difference.
- Non-intubated patients: 11% high-titer vs. 14% low-titer.
- Non-intubated patients <80 years treated w/in 72 hrs. of diagnosis, 6.3% high-titer vs. 11.3% low-titer (P = 0.0008).
Analysis of 3082 patients / 35,322 who received plasma by 4 July 2020 via Mayo Clinic’s parallel Expanded Access Program, developed to provide broader access to CP yet NOT designed to generate definitive safety or efficacy data as no untreated control group.
- 30-day mortality 29.1% in low-titer group vs. 24.7% in the high-titer group (not statistically significant).
- Suggestion that high-titer plasma beneficial when administered within 72 hours of Dx.
- 7-day mortality following high-titer vs. low-titer plasma
- COVACTA trial raises questions about tocilizumab’s benefit in COVID-19. 9/9/20. Furlow B. Lancet Rheumatol.
IL-6 has both pro-inflammatory (e.g. “cytokine storm”) and anti-inflammatory effects. Retrospective studies suggested that the IL-6 antagonist tocilizumab reduced mortality. On July 29, 2020, Hoffmann-La Roche announced results of COVACTA, a Phase 3 tocilizumab randomized controlled trial in severe COVID-19 pneumonia. Tocilizumab failed to meet the primary endpoint of improved clinical status or mortality. However, treated patients spent a week less in the hospital. The full results await publication. Proper timing of administration assessing clinical signs of hyperinflammation may prove crucial. The results of the much larger tocilizumab RECOVERY trial are pending. - Detection of SARS-CoV-2 with SHERLOCK One-Pot Testing. 9/16/2020. Joung J. N Engl J Med.
Both CRISPR (clustered regularly interspaced short palindromic repeats)- based diagnostic tests and SHERLOCK (specific high-sensitivity enzymatic reporter unlocking) can detect viruses, but are not practical for Point of Care testing. The newly described “STOPCovid.v2” (SHERLOCK Testing in One Pot version-2) uses a novel magnetic bead RNA extraction with loop-mediated isothermal amplification and CRISPR-mediated detection, all in 15-45 minutes using minimal equipment and available reagents. Nasal swab testing showed a sensitivity of 93.1% and a specificity of 98.5%. STOPCovid.v2 false negative samples had RT-qPCR Ct values greater than 37. STOPCovid.v2 detected a viral load 1/30th detected by RT-qPCR. - High Frequency of SARS-CoV-2 RNAemia and Association With Severe Disease. 9/23/20. Hogan CA. Clin Infect Dis.
Paired nasopharyngeal and plasma samples from 85 COVID-19 patients, median age 55, revealed plasma RNAemia in 28/85 (32.9%), including 22/28 (78.6%) who required hospitalization, and older age (63 vs. 50 years; P = .04). In models adjusted for age, RNAemia was more frequent in individuals who developed severe disease including ICU admission (32.1% vs 14.0%; P = .04), invasive mechanical ventilation (21.4% vs. 3.5%; P = .02), and all 4 deaths. Plasma RNA persisted for a maximum of 10 days. Authors suggest potential utility as a prognostic indicator. - High Potency of a Bivalent Human VH Domain in SARS-CoV-2 Animal Models. 9/4/2020. Li W. Cell.
Using a phage-generated library, these investigators found spike glycoprotein (S) -receptor binding domain-avid high-affinity VH binder ab8. Bivalent VH, VH-Fc ab8, bound with high avidity to S and to patient-derived S-mutants. VH-Fc ab8 was markedly effective as a prophylactic and a therapeutic, interfering in ACE-2 binding in a mouse-adapted SARS-CoV-2 and in a hamster model. The potency was enhanced by its relatively small size vs. a complete antibody (80 vs. 150 kDa). S-specificity was shown; VH-Fc ab8 did not aggregate and did not bind to 5,300 human membrane-associated proteins. These data provide a strong rationale for its therapeutic evaluation. - Reduced Monocytic Human Leukocyte Antigen-DR Expression Indicates Immunosuppression in Critically Ill COVID-19 Patients. 9/14/20. Spinetti T. Anesth Analg.
Major histocompatibility complex (MHC) Class II molecules present processed extracellular proteins and are only expressed on the surface of “professional” antigen presenting cells such as dendritic cell and macrophages/monocytes. As such, there are clear implications for SARS-CoV-2. This small monocentric prospective study examined CD14+ monocytic HLA-DR (mHLA-DR) expression in 9 ICU vs. 7 non-ICU hospitalized COVID-19 patients. The investigators found on flow cytometry significant downregulation of surface expression of this marker indicating immunosuppression. The decrease found on ICU admission persisted on days 3 and 5. The authors suggest that immune monitoring in the ICU could indicate who might benefit from immunological intervention (e.g. GM-CSF, IFNγ).
October 2, 2020:
- Association of Race and Ethnicity With Comorbidities and Survival Among Patients With COVID-19 at an Urban Medical Center in New York. 9/25/2020. Kabarriti R. JAMA Netw Open.
Among 5902 patients with positive COVID-19 diagnosis treated at a single academic center in urban New York, non-Hispanic Black and Hispanic patients had a higher proportion of more than 2 medical comorbidities and were more likely to require inpatient hospitalization, but had outcomes including mortality that were at least as good as, and maybe even marginally superior to, their non-Hispanic White counterparts when controlling for age, sex, and comorbid conditions at presentation. - Association of Red Blood Cell Distribution Width With Mortality Risk in Hospitalized Adults With SARS-CoV-2 Infection. 9/23/20. Foy BH. JAMA Netw Open.
Review of 1641 COVID-19 patients from the Boston Partners Health System found that increased red blood cell distribution width (RDW) at admission was associated with increased in-hospital mortality by multivariate analysis (ROR of 2.7) and correlated with the presence and degree of increased RDW. This effect was increased with age and an increase in RDW over the hospitalization also correlated with mortality. This finding is not novel but is simple, easily accessible and useful. This test is part of the routine complete blood count with differential that is available worldwide. - Biomarkers for the prediction of venous thromboembolism in critically ill COVID-19 patients. 9/14/20. Dujardin RWG. Thromb Res.
These authors present a prediction model for venous thromboembolism (VTE) in critically ill COVID-19 patients. They studied 127 adult patients with confirmed infection admitted to the intensive care unit. Testing included daily liver and renal function, and C-reactive protein (CRP). Twice weekly D dimer, fibrinogen, and antithrombin levels were done. Weekly duplex scans in all, and chest CT done based on clinical suspicion. The probability of a VTE with a D dimer greater than 15,000 ng/ml and a CRP greater than 280 was 98%. Hypoxemia and other variables were not predictive. Study suggests inflammation is a driving force for the development of VTE. - Patterns of COVID-19 testing and mortality by race and ethnicity among United States veterans: A nationwide cohort study. 9/22/2020. Rentsch CT. PLoS Med.
This article presents a nationwide VA data set study (~6 million patients, February 8 to July 22) comparing positive COVID-19 test results with 30-day mortality. Healthcare disparities were explored by evaluating “associations between race/ethnicity and receipt of COVID-19 testing, a positive test result, and 30-day mortality, with multivariable adjustment for demographic and clinical characteristics including comorbid conditions, health behaviors, medication history, site of care, and urban versus rural residence.” The study confirms prior reports indicating that “Black and Hispanic individuals experience excess burden of SARS-CoV-2 infection” but not increased mortality and notes that these disparities “are not entirely explained by underlying medical conditions or where they live or receive care.” The article contains interesting distinctions and reinforces the importance of designing “strategies to contain and prevent further outbreaks in racial and ethnic minority communities.” - Practical strategies to reduce nosocomial transmission to healthcare professionals providing respiratory care to patients with COVID-19. 9/24/20. Kaur R. Crit Care.
The authors of this well-illustrated review article discussed protecting healthcare workers from infection due to contacts with COVID-19 patients. The authors provide practical, step-by-step strategies to reduce aerosols during respiratory interventions. Authors provide an excellent summary of respiratory care with tables and pictures for the safety of healthcare workers. - Racial Disparities in Incidence and Outcomes Among Patients With COVID-19. 9/25/2020. Muñoz-Price LS. JAMA Netw Open.
This article investigates the goal-described patterns and outcomes of COVID-19 by race, controlling for age, sex, socioeconomic status, and comorbid conditions among 2595 urban patients. COVID-19 positivity was associated with Black race. Among patients with COVID-19, both race and poverty were associated with higher risk of hospitalization, but only poverty was associated with higher risk of intensive care unit admission. The findings also imply that adverse outcomes and greater population mortality associated with Blacks early in the course of the US pandemic were primarily attributable to greater incidence of COVID-19 among African American residents rather than worse survival once hospitalized. - Reducing the Risk and Impact of Brachial Plexus Injury Sustained From Prone Positioning-A Clinical Commentary. 9/22/20. Simpson AI. J Intensive Care Med.
This is a commentary from the UK based on a literature review of the prevention and approach toward brachial plexus injuries in proned patients. Six positioning suggestions are made to prevent common traction and compression injuries, and an algorithm is presented on how to evaluate for and triage brachial plexus injuries. The bottom line is that there is no foolproof way to protect the brachial plexus, and “frequent, careful and deliberate changing of position is the main method to reduce injury.” - Risk factors associated with adverse fetal outcomes in pregnancies affected by Coronavirus disease 2019 (COVID-19): a secondary analysis of the WAPM study on COVID-19. 9/25/20. Di Mascio D. J Perinat Med.
This is a small sample article which labels COVID-19 infection in first trimester as associated with “adverse perinatal outcomes.” A high cesarean delivery rate of over 50% and a 4% neonate mortality are listed although no control statistics for comparison are provided. - Risk Factors for Hospitalization, Mechanical Ventilation, or Death Among 10 131 US Veterans With SARS-CoV-2 Infection. 9/23/2020. Ioannou GN. JAMA Netw Open.
This large study showed no increase in mortality associated with Black or Hispanic race, obesity, COPD, hypertension or smoking (contrary to what has been found in smaller, prior studies). It did find the expected association of increased severity and mortality with older age (≥50) and multiple comorbidities. - SARS-CoV-2 Infection Among Hospitalized Pregnant Women: Reasons for Admission and Pregnancy Characteristics – Eight U.S. Health Care Centers, March 1-May 30, 2020. 9/25/20. Panagiotakopoulos L. MMWR Morb Mortal Wkly Rep.
This Vaccine Safety Datalink (VSD) surveillance program studied hospitalized pregnant patients (n= 105; OB-62 pregnant women with SARS-CoV-2 infection who were asymptomatic vs. 43 who were symptomatic). COVID-19 was identified in higher rates of complications in pregnant women with infection due to changes in immunity/respiratory compromise, exaggeration of comorbidities leading to adverse outcome in pregnancy, ICU admission, and death. This article highlights the importance of all pregnant women attending antenatal care irrespective of insurance coverage and follow general guidelines. There’s a nice infographic showing that hospitalized pregnant women with COVID-19 can have severe illness. - Sensitive Detection of SARS-CoV-2-Specific Antibodies in Dried Blood Spot Samples. 9/24/20. Morley GL. Emerg Infect Dis.
Dried blood spot (DBS) samples can be obtained directly from patients without venipuncture and stored and shipped without refrigeration. DBS samples were compared to matched serum samples in 80 patients to detect coronavirus 2 spike antibodies with a relative 98.1% sensitivity and 100% specificity. The authors propose that DBS sampling offers an alternative for population-wide serologic testing in the coronavirus pandemic.
September 30, 2020:
- New Studies on COVID-19 Epidemiology
The following four articles examine risk factors for developing COVID-19, for having severe disease and for death. Common findings include an increased risk of infection and hospitalization in Blacks but no increase in mortality. It should be noted that the mentioned hospitalization rates may depend on socio-economic factors and may not be a clear indicator of severity of disease.- Patterns of COVID-19 testing and mortality by race and ethnicity among United States veterans: A nationwide cohort study. 9/22/20. Rentsch CT. PLoS Med.
This article presents a nationwide VA data set study (~6 million patients, February 8 to July 22) comparing positive COVID-19 test results with 30-day mortality. Healthcare disparities were explored by evaluating “associations between race/ethnicity and receipt of COVID-19 testing, a positive test result, and 30-day mortality, with multivariable adjustment for demographic and clinical characteristics including comorbid conditions, health behaviors, medication history, site of care, and urban versus rural residence.” The study confirms prior reports indicating that “Black and Hispanic individuals experience excess burden of SARS-CoV-2 infection” but not increased mortality and notes that these disparities “are not entirely explained by underlying medical conditions or where they live or receive care.” The article contains interesting distinctions and reinforces the importance of designing “strategies to contain and prevent further outbreaks in racial and ethnic minority communities.” - Risk Factors for Hospitalization, Mechanical Ventilation, or Death Among 10 131 US Veterans With SARS-CoV-2 Infection. 9/23/20. Ioannou GN. JAMA Netw Open.
This large study showed no increase in mortality associated with Black or Hispanic race, obesity, COPD, hypertension or smoking (contrary to what has been found in smaller, prior studies). It did find the expected association of increased severity and mortality with older age (>50) and multiple comorbidities. - Association of Race and Ethnicity With Comorbidities and Survival Among Patients With COVID-19 at an Urban Medical Center in New York. 9/25/20. Kabarriti R. JAMA Netw Open.
Among 5902 patients with positive COVID-19 diagnosis treated at a single academic center in urban New York, non-Hispanic Black and Hispanic patients had a higher proportion of more than 2 medical comorbidities and were more likely to require inpatient hospitalization, but had outcomes including mortality that were at least as good as, and maybe even marginally superior to, their non-Hispanic White counterparts when controlling for age, sex, and comorbid conditions at presentation. - Racial Disparities in Incidence and Outcomes Among Patients With COVID-19. 9/25/20. Muñoz-Price LS. JAMA Netw Open.
This article investigates the goal-described patterns and outcomes of COVID-19 by race, controlling for age, sex, socioeconomic status, and comorbid conditions among 2595 urban patients. COVID-19 positivity was associated with Black race. Among patients with COVID-19, both race and poverty were associated with higher risk of hospitalization, but only poverty was associated with higher risk of intensive care unit admission. The findings also imply that adverse outcomes and greater population mortality associated with Blacks early in the course of the US pandemic were primarily attributable to greater incidence of COVID-19 among African American residents rather than worse survival once hospitalized.
- Patterns of COVID-19 testing and mortality by race and ethnicity among United States veterans: A nationwide cohort study. 9/22/20. Rentsch CT. PLoS Med.
- Cardiopulmonary exercise and the risk of aerosol generation while wearing a surgical mask. 9/11/20. Helgeson SA. Chest.
The authors quantified the number of various-sized airborne particles 6 feet from exercising normal volunteers wearing type II procedural surgical masks. They found there was a minimal increase of particle number at low and moderate exercise but a doubling of the ambient baseline of small respirable particles (0.3–0.5 micrometer) with very hard exercise. Larger droplet sized particles were not significantly increased during any stage of exercise. These results may be applicable to gyms and health clubs if all participants wear surgical masks. - Occurrence and transmission potential of asymptomatic and presymptomatic SARS-CoV-2 infections: A living systematic review and meta-analysis. 9/22/20. Buitrago-Garcia D. PLoS Med.
Ninety-four reviewed studies identified from 25 March through 10 June 2020:
- ~20% remain asymptomatic when infected with SARS-CoV-2 (79 studies); 31% in screened populations (7 studies).
- Compared with symptomatic contacts, relative risk of transmission from asymptomatic contacts = 0.35 (95% CI 0.10–1.27); from presymptomatic contacts = 0.63 (95% CI 0.18–2.26).
- “Easing of restrictions will only be possible with wide access to testing, contact tracing, and rapid isolation of infected individuals.” Prevention measures (enhanced hand hygiene, masks, social distancing) and quarantine of close contacts are essential to prevent onward transmission during asymptomatic or presymptomatic periods.
- SARS-CoV-2-Associated Deaths Among Persons Aged <21 Years – United States, February 12-July 31, 2020. 9/18/20. Bixler D. MMWR Morb Mortal Wkly Rep.
This CDC Morbidity and Mortality Weekly Report describing deaths in <21 year old population. Most patients are Hispanic or Black, and 45% had 2 or more associated illnesses. Most of the deaths occurred in 18-20 year olds. Of curiosity, only 8% exhibited the inflammatory illness possibly due to the large number that died out-of-hospital or in the ER. Most significant is that although 391,814 cases were reported in the age group, only 121 deaths occurred, a fatality rate of 0.08%.
September 25, 2020:
- Association of Daily Wear of Eyeglasses With Susceptibility to Coronavirus Disease 2019 Infection. 9/16/20. Zeng W. JAMA Ophthalmol.
While the public has not received guidance to wear eye protection to decrease the risk of COVID-19, Zeng raised the question of whether ordinary eyeglasses may help prevent infection, as in their observational study of 276 COVID-19 inpatients of which only 5.8% wore glasses vs. 31.5% in a reference population. This editorial highlights the study’s weaknesses, including that the “local population” data were from another region of China and another time period altogether. Although the data are unlikely to be by chance alone, an inference of cause requires additional study. - Glucocorticoid therapy does not delay viral clearance in COVID-19 patients. 9/22/2020. Ji J. Crit Care.
This is a (LtE) retrospective observational study regarding glucocorticoids and Covid viral clearance. Out of 684 patients noted 29.5% had viral RNA clearance within 14 days after illness onset and 30.7% cases had viral RNA clearance between 14 and 28 days, and 39.8% cases had viral RNA clearance over 28 days. There were no differences on the age, gender, and underlying diseases between different groups. The degree of decrease in CD4 T cell and B cell counts on admission was related with the prolonged viral RNA clearance. The results show that GC therapy shortened hospital stay days but had no effect on the virus clearance time. This is true for the severe and critical patients as well. The GC treatment had no effect on the peripheral lymphocyte counts, including CD4 T cells, CD8 T cells, NK cells, and B cells. - COVID-19 concerns aggregate around platelets. 9/10/20. Battinelli EM. Blood.
This is a well-written, useful editorial which describes the essence of the following two papers, including its limitations and future steps. - Platelet gene expression and function in patients with COVID-19. 9/10/20. Manne B. Blood.
Using platelet RNA sequencing, this group profiles gene expression in the platelets of COVID-19 patients (n= 41) and finds altered gene expression profiles in pathways associated with ubiquitination, antigen presentation, and mitochondrial dysfunction. Patients with COVID-19 have higher levels of platelet activation at rest and increased interactions with neutrophils, monocytes, and T cells compared with healthy donors. Platelet functionality studies demonstrate hyperactivity, as evidenced by increased aggregation, spreading on fibrinogen and collagen through upregulation of the MAPK pathway, and increased thromboxane generation. These new data help extend prior data into the basic science of the hypercoagulable state of COVID-19. - Platelet activation and platelet-monocyte aggregate formation trigger tissue factor expression in patients with severe COVID-19. 9/10/20. Hottz E. Blood.
This group demonstrates that COVID-19 is associated with increased platelet activation. They show that the platelets of critically ill COVID-19 patients exhibit increased platelet aggregation and platelet-monocyte aggregation. Further, these changes correlate with a worse outcome. Changes in platelet activation were associated with increased platelet expression of P-selectin and CD63. Platelets from patients with severe COVID-19 infection induce monocyte-derived tissue factor (TF) expression that is diminished by pretreating COVID-19 patient platelets with an anti–P-selectin neutralizing antibody or the clinically approved anti-αIIb/β3 monoclonal antibody, abciximab. These data are new and add to the understanding of the role that platelets play in the hypercoagulable state of COVID-19. - Probative Value of the D-Dimer Assay for Diagnosis of Deep Venous Thrombosis in the Coronavirus Disease 2019 Syndrome. 9/15/20. Gibson CJ. Crit Care Med.
The authors tested the utility of the D-dimer assay for the diagnosis of deep vein thrombosis. Despite the excellent correlation between the D-dimer and the presence of DVT, the positive predictive value was 21.8%. DVT is only one aspect of the thrombotic problems in these patients. Many do not recommend leg duplex scanning using the sole criteria of D-dimer. One interesting aspect of this study was that all ICU patients received therapeutic anticoagulation. That may have been reflected in the low incidence of DVT discovered in these patients. Unfortunately, there are no data presented regarding the incidence of bleeding in these patients. - Stroke Risk, phenotypes, and death in COVID-19: Systematic review and newly reported cases. 9/15/20. Fridman S. Neurology.
This is a complex study of stroke characteristics in COVID-19 patients by an international team of neurologists who pooled results from 10 studies with their own case series for a total of 160 patients. Their goal is to estimate overall incidence of stroke (1.8%) and mortality (34.4%), determine risk factors, particularly in patients under age 50, and identify clinical phenotypes and associated mortality separating all strokes from ischemic etiology. Large vessel occlusion contributed to a high percentage of strokes in younger patients and occurred before the onset of COVID-19 symptoms in 49% of those cases, while pulmonary involvement correlated with strokes in older patients and poor outcomes.
September 23, 2020:
- Bridging the Gap at Warp Speed – Delivering Options for Preventing and Treating Covid-19. 9/15/20. Slaoui M. N Engl J Med.
This article summarizes ongoing initiatives by industry and the Departments of Defense and HHS to develop and distribute novel therapeutics safely and effectively by the end of 2020. Under the code name Operation Warp Speed (OWS), teams are focused on:- Creating passive immunity using convalescent plasma, hyperimmune globulin and monoclonal antibodies (mAbs);
- Inhibiting viral replication using new and repurposed antivirals like remdesivir;
- Prevention of disease in high-risk cohorts applying neutralizing mAbs; and
- Developing novel immunomodulators and anticoagulants.
OWS plans to attack COVID-19 using some of these options before an anticipated vaccine release in early 2021. The article does not address the progress of ongoing vaccine development efforts by OWS.
- Coronavirus Disease 2019 and Acute Respiratory Distress Syndrome: Why the Intensivist Is More Important Than Ever. 9/15/20. Cereda M. Crit Care Med.
This article provides an excellent discussion combining diplomacy with clinical and scientific observation to reconcile interpretational differences of variable COVID-19 pulmonary presentations. While not undermining traditional ARDS management but instead illuminating and describing potential discrepancies, the authors present a timely reassessment of COVID-19 pulmonary presentations. They underscore need for continued research and investigation into pathophysiology and individualized and timely intervention depending upon clinical presentation. - Guiding Principles for the Conduct of Observational Critical Care Research for Coronavirus Disease 2019 Pandemics and Beyond: The Society of Critical Care Medicine Discovery Viral Infection and Respiratory Illness Universal Study Registry. 9/15/20. Walkey AJ. Crit Care Med.
The article describes developed guiding principles for use of observational data. Topics covered include research workforce and infrastructure, rapid, harmonized data collection, processes for choosing research questions, state-of-the-art observational methods, accounting for random error, innovative peer-review pathways, and implementation/improvement. It is likely to be a valuable, timely tool during the current pandemic and beyond. - Healthcare professionals’ perceptions of critical care resource availability and factors associated with mental well-being during COVID-19: Results from a US survey. 9/2/20. Sharma M. Clinical Infectious Dis.
This is a report of survey data regarding the psychological well-being of 1651 ICU workers from all 50 states. With extensive statistical analysis, tables and graphs, authors document higher relative rates of emotional distress and burnout associated with insufficient PPE (1.43), stigma from community (1.32) and poor communication from supervisors (1.13). Conclusion: addressing these issues along with effective, periodic communication from supervisors may improve ICU worker well-being during the COVID-19 pandemic. An accompanying, well-written editorial discusses the psychological importance to healthcare workers of adequate PPE, and of human relationships and trust among supervisors, workers and the community. - Lung ultrasonography for risk stratification in patients with COVID-19: a prospective observational cohort study. 9/17/20. Brahier T. Clin Infect Dis.
This article presents the results of a prospective, blinded study of 80 RT-PCR+ patients in Switzerland who underwent lung ultrasound on presentation in the Emergency Department. The extent and nature of the lung pathology showed a significant predictive relationship with the severity of COVID-19 pneumonia 7 days later. This study, including both in- and out-patients, reinforces previously noted utility, such as the finding that 9 of 10 patients with a normal CXR had an abnormal lung ultrasound, including one who later died. - Risk Factors for COVID-19-associated hospitalization: COVID-19-Associated Hospitalization Surveillance Network and Behavioral Risk Factor Surveillance System. 9/18/2020. Ko JY. Clin Infect Dis.
Well-conducted study including 5,416 confirmed COVID-19 patients comparing hospitalized patients identified from the COVID-19-Associated Hospitalization Surveillance Network (COVID-NET) cataloguing hospital admissions with the Behavioral Risk Factor Surveillance System, a telephone survey instrument which identifies populations of interest (co-morbidities previously reported as increased risk for disease severity and outcome; e.g. age, hypertension, diabetes, etc.). Extensive statistical analysis and well-written discussion summarized: “Severe obesity, chronic kidney disease, diabetes, obesity, hypertension, asthma, age ≥45, male sex, and non-Hispanic black and other race/ethnicity are associated with increased risk of COVID-19-associated hospitalizations.” - Severe COVID-19 Infections—Knowledge Gained and Remaining Questions. 9/18/20. Bos LDJ. JAMA Intern Med.
This editorial provides a brief, balanced and valuable overview of current best therapies for COVID-19-associated ARDS as informed by recent scientific literature. It also discusses therapies (e.g., hydroxychloroquine, lopinavir/ritonavir and IL-6 blockers) for which there was initial hope based on lab findings or “theoretical understandings of disease pathogenesis,” that have subsequently been shown by randomized, controlled studies to have no significant value. Authors caution clinicians to be patient and base treatment on prospective, controlled trials as they become available. - The role of fit testing N95/FFP2/FFP3 masks: a narrative review. 9/15/20. Regli A. Anaesthesia.
Fit testing confirms which respirator model provides adequate respiratory protection to an individual. Required to comply with respirator standards, fit testing is costly and not consistently performed. Quantitative fit testing is superior to qualitative fit testing; however, the tested respirator is discarded as it is punctured. Fit checking by the wearer is not a reliable substitute, although strongly recommended with each respirator donning. The role of potential aerosol transmission of SARS-CoV-2 is an area of active research and debate. N95 or higher-level protection is recommended for aerosol generating procedures.
September 21, 2020:
- Elevated D-dimers and lack of anticoagulation predict PE in severe COVID-19 patients. 9/9/20. Mouhat B. Eur Respir J.
This article reviews 162 patients who had computed tomography pulmonary angiography (CTAP) with clinical pulmonary deterioration taken from 349 patients with COVID-19 in a French hospital. Twenty-seven percent had pulmonary embolism (PE). Review of their data with multivariate analysis demonstrates lack of anticoagulation and D-dimer > 2590 ng/ml to be predictive of PE. A D-dimer level >2590 ng/mL−1 was associated with a 17-fold increase (!), and lack of anticoagulation with a 4-fold increase in the risk of PE. Linearity was verified for D-dimers in the study population (test of linearity <0.001). This paper adds more details to the literature and helps guide the clinician. - Favorable outcomes of COVID-19 in recipients of hematopoietic cell transplantation. 9/8/20. Shah GL. J Clin Invest.
From Sloan Kettering, a retrospective study of 77 COVID-19 PCR+ recipients of allogeneic and autologous hematopoietic cell transplant and chimeric antigen receptor T cell therapy (44% admitted). Of the 77 cellular therapy recipients, the results were: Allo = 35, Auto = 37, CAR-T = 5. The median time from cellular therapy was 782 days. Overall survival at 30 days was 78%. Clinical variables significantly associated with more severe disease (greater than non-rebreathing mask oxygen) or death were number of comorbidities, infiltrates and neutropenia. Worsening graft-versus-host-disease was not identified. The authors observed rapid recovery in lymphocyte populations across lymphocyte subsets which are critical to anti-viral responses and immune reconstitution. - Neurological and neuropsychiatric complications of COVID-19 in 153 patients: a UK-wide surveillance study. 6/25/20. Varatharaj A. Lancet Psychiatry.
Report on a nationwide, cross-specialty surveillance study of acute neurological and psychiatric complications of COVID-19 in the UK combined with a call for similar initiative to collect data on short- and long-term neurological and psychiatric sequelae of COVID-19 worldwide. The authors used a secure rapid-response case report notification portal that was made available to all pertinent professional organizations and obtained valuable and timely data to be reviewed by clinicians, researchers and funders. - Racial/Ethnic Variation in Nasal Gene Expression of Transmembrane Serine Protease 2 (TMPRSS2). 9/10/20. Bunyavanich S. JAMA.
Nasal epithelium contains a protease (transmembrane serine protease 2 – TMPRSS2) which facilitates SARS-CoV-2 virus entry into the body. In a racially diverse cohort participating in an asthma study between 2015 – 2018, Black individuals exhibited a significantly higher expression of TMPRSS2 in nasal epithelium compared with other self-identified races/ethnicities. This finding may shed further light on the observed higher burden of COVID-19 among Black individuals. Protease inhibitors, like camostat mesylate, are undergoing clinical trials to test their utility for COVID-19 treatment via TMPRSS2 inhibition. - The coronavirus is mutating – does it matter? 9/8/20. Callaway E. Nature.
In an article from Nature, mutations in the SARS-CoV-2 are reviewed. Mutations in RNA viruses such as SARS-CoV-2 containing “proofreading” enzymes occur slowly. One distinct mutation in the spike protein gene occurs at the 614th amino-acid position: the aspartate (D, in biochemical shorthand) is replaced by glycine (G) in the virus’s 29,903-letter RNA code. The “D614G mutation” became the dominant SARS-CoV-2 lineage in Europe and the US. Despite early alarm, it does not enhance spread or affect antibody defense. More than 12,000 mutations in SARS-CoV-2 are catalogued. The author speculates that worrisome mutations could arise especially if antibody therapies producing selection pressure are not used wisely.
September 16, 2020:
- Azithromycin for severe COVID-19. 9/4/20. Oldenburg CE. Lancet.
This is a commentary on the Brazilian Coalition II trial comparing the addition of azithromycin to standard of care which included hydroxychloroquine on outcome; no benefit was detected. The authors then discuss relevance of the earlier Coalition I study conducted by the same authors which compared use of hydroxychloroquine with or without azithromycin and showed no increase in complications and no therapeutic benefit. Combined results confirm other evidence that combination of azithromycin with hydroxychloroquine conveys no benefit; the results suggest eliminating azithromycin to decrease antibiotic overuse unless culture relevance determined or evidence of superinfection. - Azithromycin in addition to standard of care versus standard of care alone in the treatment of patients admitted to the hospital with severe COVID-19 in Brazil (COALITION II): a randomised clinical trial. 9/4/20. Furtado RHM. Lancet.
Randomized, multi-center, open-label Brazilian trial designed to test whether addition of azithromycin to the standard of care, which included hydroxychloroquine, improved clinical outcomes in patients with confirmed COVID-19 diagnosis. Carefully controlled and conducted study with negative outcome indicating that azithromycin added to hydroxychloroquine conveyed no benefit. Small signal of increased morbidity in younger patients. - Bacterial and viral co-infections in patients with severe SARS-CoV-2 pneumonia admitted to a French ICU. 9/7/2020. Contou D. Ann Intensive Care.
In this retrospective single center study, 92 patients were cultured within 48 hours of admission to the ICU. Twenty-eight percent of these patients were culture positive for bacteria, and as the authors state in their discussion “might” have had a respiratory bacterial co-infection upon ICU admission. The leading involved bacteria were methicillin-sensitive Staphylococcus aureus (31%), Streptococcus pneumoniae (22%), Haemophilus influenzae (19%) and Enterobacteriaceae (16%) with no infection related to atypical bacteria and no viral co-infection especially no influenza infection. - Facial Masking for Covid-19 — Potential for “Variolation” as We Await a Vaccine. 9/8/20. Gandhi M. N Engl J Med.
This opinion piece presents evidence that wearing a face mask may reduce the viral inoculum the wearer receives thereby reducing COVID-19 infection symptoms. Results from animal models and comparisons of outbreaks on cruise ships and in processing plants with and without mask use support conclusions. In addition to protecting others, masking may reduce the rate and severity of new infections for mask wearers. - High Concentrations of Nitric Oxide Inhalation Therapy in Pregnant Patients With Severe Coronavirus Disease 2019 (COVID-19). 8/26/20. Fakhr B. Obstetrics & Gynecology.
Inhalational nitric oxide (NO) at 160-200 ppm (high dose) for 30-60 minutes twice daily was administered to 6 pregnant women with severe-critical COVID-19 respiratory dysfunction. All improved clinically. Methemoglobin levels peaked at 2.5%. An additional 4 of 6 patients received continuous low-dose NO during periods of intubation or during vaginal delivery. One mother, who had respiratory distress, delivered twins at 30 weeks by cesarean delivery and later developed transient acute kidney injury. No other adverse effects were observed. The authors referenced studies reporting NO to be anti-viral. One author reports corporate support; see article. - Increased Odds of Death for Patients with Interstitial Lung Disease and COVID-19: A Case-Control Study. 9/8/2020. Esposito AJ. Am J Respir Crit Care Med.
This letter to the editor compares the COVID-19 mortality rate in a group of 42 PCR positive patients with previously diagnosed interstitial lung disease (ILD) to a group of matched PCR positive controls. Mortality was 33% in the patients with ILD and 13% in the matched controls. Increased mortality was observed even after adjustment for age, sex, race, smoking status, cardiovascular disease (congestive heart failure and/or coronary artery disease), and any chronic immunosuppression. - Prognostic Value of Elevated Cardiac Troponin I in Hospitalized Covid-19 Patients. 8/27/20. Shah P. Am J Cardiol.
Elevated troponins were found in a significant number of COVID-19 positive patients admitted to hospital. Elevated levels were predictive of increasing disease severity and poor outcome. - Risk stratification of patients admitted to hospital with covid-19 using the ISARIC WHO Clinical Characterisation Protocol: development and validation of the 4C Mortality Score. 9/10/20. Knight SR. BMJ.
Observational study utilizing the Coronavirus Clinical Characterization Consortium Mortality Score (Model-4C) to assess mortality in two groups of COVID-19 patients, using health data from 260 UK hospitals. Both groups demonstrated 32.2% mortality (February to May, N= 35,463 and May to June, N=22,361). The Model-4C Mortality Score incorporates 8 clinical admission criteria: age, sex, number of comorbidities, respiratory rate, peripheral oxygen saturation, level of consciousness, urea level, and C reactive protein. The score showed high discrimination for mortality with an ROC of 0.79. Relevant statistics, graphs and tables are included in the article. - Time-critical goals of care in the Emergency Department during COVID-19: A three-stage protocol. 6/17/20. Nakagawa S. Journal of the American Geriatric Society.
This is an important and ethically relevant research letter discussing applicability of initiating palliative care discussions in the Emergency Department (ED) and defining a “clear goal of care” in this COVID-19 pandemic. The author proposes a simple 3-stage communication approach (1. sharing knowledge, 2. clarifying goal of care, and 3. negotiating treatment options) with the patient’s family and ED physicians that allows clinicians to quickly share the clinical picture, effectively assess the patient’s values, and make a goal recommendation for care during our rapidly progressing crisis. The 3-stage tool is very practical and saves resources while preserving the patient’s autonomy and wishes.
September 14, 2020:
- Association of Treatment Dose Anticoagulation With In-Hospital Survival Among Hospitalized Patients With COVID-19. 6/29/20. Paranjpe I. JACC.
The authors studied 2,773 hospitalized patients with COVID-19. Therapeutic anticoagulation was administered to 28% of these patients and survival between those who received prophylactic versus therapeutic anticoagulation was similar. In patients who required mechanical ventilation who received treatment doses of anticoagulation, in-hospital mortality rates were lower. Bleeding was more common for intubated patients. Prospective randomized trials will be needed to confirm these findings but the results in this study are very encouraging. These preliminary results provide some guidance for selecting therapeutic heparin in critical situations. - Coagulation biomarkers are independent predictors of increased oxygen requirements in COVID-19. 8/17/20. Rauch A. J Thromb Haemost.
This well-done study from Lille, France of 234 patients admitted with COVID-19 presents new data. von Willebrand factor (VWF) levels were associated with severity and oxygen need in COVID-19 at admission; low factor VIII (FVIII)/VWF ratio at admission is predictive of increased oxygen requirements; and coagulation biomarkers predict outcome independently of major comorbidities in COVID-19. Furthermore, FVIII is predictive of early thrombotic events irrespective of BMI in COVID-19. - COVID-19: more than a cytokine storm. 9/5/20. Riva G. Crit Care.
This commentary from Modena, Italy cites the current overemphasis on therapies combating the cytokine storm of the innate COVID-19 immune response and “neglect” of fighting the adaptive immune response. Lymphocyte dysregulations in COVID-19 include lymphopenia (CD4+ and CD8+), T cell exhaustion and a skewing toward a low IFN-Ɣ CD4+ tolerogenic balance. Some of these adaptive deficiencies also are evident in cancer and with aging. The authors advocate trials with immunotherapeutic drugs that may reverse T cell impairment. Trials to determine appropriate immunomodulatory drugs, antibodies, biomarkers and their optimal timing are beginning. - Effect of Remdesivir vs Standard Care on Clinical Status at 11 Days in Patients With Moderate COVID-19. 8/21/20. Spinner C. JAMA.
In this international study (United States, Europe, and Asia) of COVID-19 patients with pulmonary infiltrates but oxygen saturation above 94% (moderate COVID-19 pneumonia), patients who received a 5-day course of remdesivir did better on day 11 than a comparable group of patients who received standard care only. However, a 10-day course of remdesivir failed to show clinical improvement compared to standard care. The results suggest that remdesivir works when given early and may not have additional benefit once patients progress to more severe illness. - Non-neuronal expression of SARS-CoV-2 entry genes in the olfactory system suggests mechanisms underlying COVID-19-associated anosmia. 7/31/20. Brann DH. Science Advances.
The authors examined human and mouse olfactory epithelial cells and found ACE2 is expressed not in olfactory neurons but in dorsally located olfactory epithelial sustentacular cells and olfactory bulb pericytes support cells, goblet and ciliated cells, stem cells, and perivascular cells. Hence, neurons are not injured and the findings suggest that sensory damage is unlikely to be permanent and should usually recover within a few weeks. - Perspective of the Surviving Sepsis Campaign on the Management of Pediatric Sepsis in the Era of Coronavirus Disease 2019. 9/4/20. Weiss SL. Pediatr Crit Care Med.
The authors provide a framework for the early recognition and initial resuscitation of children with sepsis or septic shock caused by all pathogens. The emphasis of COVID-19 has more in common with other forms of sepsis than was originally appreciated; 6 key managements are listed: IV (if necessary, intraosseous); blood culture; broad spectrum antimicrobials; measure lactate, fluid boluses for shock if needed; and start vasoactive drugs if shock persists. - Safety Update: COVID-19 Convalescent Plasma in 20,000 Hospitalized Patients. 7/19/20. Joyner MJ. Mayo Clin Proc.
This was a study based on a collaborative effort of the FDA, Mayo Clinic and the national blood banking community. Over 20,000 patients received convalescent plasma in the US. In this report of 20,000 patients, the one week mortality was 13%; transfusion reactions were <1% (n=78). This is important data supporting the use of convalescent plasma. However, these data examined the safety of its use not the efficacy. While these data are important, we will be looking forward to further information in the future. - Subcutaneous Enoxaparin Safely Facilitates Bedside Sustained Low-Efficiency Hemodialysis in Hypercoagulopathic Coronavirus Disease 2019 Patients-A Proof-of-Principle Trial. 7/23/2020. Neumann-Haefelin E. Crit Care Explor.
Faced with recurrent filter clotting and incomplete dialysis in hypercoagulable COVID-19 patients needing renal replacement therapy, these authors changed therapeutic anticoagulation from unfractionated heparin to low molecular weight heparin. In their retrospective study of 3 patients, LMWH markedly increased successful completion of RRT. Their protocol reduces the risk of discarding important resources, filter and blood and at the same time provides adequate dialysis quality. - The Effect of Ultraviolet C Radiation Against Different N95 Respirators Inoculated with SARS-CoV-2. 8/28/20. Ozog DM. Int J Infect Dis.
This study from Michigan provides new data regarding the ability of ultraviolet (UV)-C to inactivate SARS-CoV-2 on specific N95 respirator models. A dose of 1.5 J/cm2 to each mask side was adequate for 3M 1860 and Moldex 1511. Straps of 3M 1860 required secondary decontamination. Three other models tested had residually detectable virus when cultured, confirming model-dependent heterogeneity and need for secondary strap decontamination found in previous studies. No fit testing was done. Implementation of UV-C decontamination of N95 respirators requires careful consideration of model, material type, design, and fit-testing following irradiation. - The Respiratory Drive: An Overlooked Tile of COVID-19 Pathophysiology. 9/4/2020. Gattinoni L. Am J Respir Crit Care Med.
This editorial reviews a French paper (https://www.atsjournals.org/doi/abs/10.1164/rccm.202005-1582LE, in IARS Newsletter 14) that investigated the usefulness of measuring respiratory drive in COVID-19 patients being weaned from mechanical ventilation, and showed that patients with high respiratory drive are more likely to fail weaning and extubation. The editorial speculates that routinely measuring respiratory drive might be useful, and discusses possible physiologic mechanisms for the paradox of high minute ventilation and low rapid shallow breathing index in COVID patients with high compliance.
September 9, 2020:
- Acute kidney injury in patients with SARS-CoV-2 infection. 9/3/20. Joseph A. Ann Intensive Care.
French authors noted COVID-19 reports lacked consistent definitions of AKI. Using the standardized Kidney Disease Improving Global Outcomes (KDIGO) criteria in a retrospective study of 100 COVID-19 ICU patients, they found 81% had AKI and 35% died at 28 days (vs. 1%), higher than previously reported. 90% who died with AKI were intubated; 50% required vasopressors. Relative risk of AKI was 1.3 for each adjusted SOFA score point. AKI was not independently associated with PEEP levels, complement activation, fibrinogen or inflammatory markers. 28-day Kaplan–Meier curves without (n=19) and with (n=81) 3 stages of AKI are provided. - Anticipating and managing coagulopathy and thrombotic manifestations of severe COVID-19. 8/16/20. Godoy LC. CMAJ.
This is an interesting, informative, and well-written review. The explanation of the pathology beginning with the viral spike protein invading the cells facilitated by ACE2 followed by a cascade of reactions involving inflammatory and immunological pathways resulting in widespread endotheliitis is well stated. The clarity of the authors’ approach is refreshing. A summary of current recommendations is presented along with interesting individual studies that stimulate the reader and the researcher to pursue additional studies. It’s interesting to note that the reported bleeding rate using full anticoagulation is not much different than using lower doses. - Cardiac Surgery-Enhanced Recovery Programs Modified for COVID-19: Key Steps to Preserve Resources, Manage Caseload Backlog, and Improve Patient Outcomes. 9/1/20. Gregory AJ. J Cardiothorac Vasc Anesth.
The authors discuss modifications to cardiac ERPs given case backlogs and overlapping resource utilization requirements between cardiac surgery patients and COVID-19 patients. The discussion includes specific metrics as well as an overview of organizational approaches relevant to the COVID-19 environment. Adaptations are likely to influence care models beyond the pandemic and concepts are applicable to a wide range of specialty care. - Saliva or Nasopharyngeal Swab Specimens for Detection of SARS-CoV-2. 8/28/20. Wyllie AL. N Engl J Med.
Self-obtained saliva samples and RN-obtained nasopharyngeal (NP) swabs were PCR tested every 3 days in 70 COVID-19 inpatients. Saliva samples were at least as sensitive as NP swabs, and showed more RNA copies. Also, 495 saliva tests from asymptomatic health care workers revealed 13 positive results. 7/9 who had concurrent self-obtained NP swabs were negative. All 13 were confirmed positive for COVID-19. These data, reported in a Letter to the Editor, support self-obtained saliva testing, if done in a carefully controlled manner. Methods are reported in supplementary data to the Letter. - Seroprevalence of SARS-CoV-2 Among Frontline Health Care Personnel in a Multistate Hospital Network – 13 Academic Medical Centers, April-June 2020. 9/4/20. Self WH. MMWR Morb Mortal Wkly Rep.
A high proportion of SARS-CoV-2 infections among health care personnel appear to go undetected. Of 3248 personnel observed, 6% had antibody evidence of previous SARS-CoV-2 infection; 29% of personnel with SARS-CoV-2 antibodies were asymptomatic in the preceding months, and 69% had not previously received a diagnosis of SARS-CoV-2 infection. Prevalence of SARS-CoV-2 antibodies was lower among personnel who reported always wearing a face covering while caring for patients (6%), compared with those who did not (9%). - The effect of coronavirus infection (SARS-CoV-2, MERS-CoV, and SARS-CoV) during pregnancy and the possibility of vertical maternal-fetal transmission: a systematic review and meta-analysis. 9/4/20. Diriba K. Eur J Med Res.
A worldwide retrospective report (biased with Chinese studies) on the effect of coronavirus in pregnancy. Includes over 100 patients with all 3 coronavirus diseases of note — SARS, MERS and COVID-19. No transmission to neonates was detected with any virus, hypothesized to be due to the lack of placental angiotensin converting enzyme 2 (ACE-2) receptors. Maternal pulmonary involvement presented the greatest complicating factor in pregnancy. Deaths were rare and mostly related to MERS infected mothers. - Update Alert 3: Risks and Impact of Angiotensin-Converting Enzyme Inhibitors or Angiotensin-Receptor Blockers on SARS-CoV-2 Infection in Adults. 8/26/2020. Mackey K. Ann Intern Med.
Report of an updated review of new literature studying association of ARB’s and ACEI’s use with severity and COVID-19 adverse outcomes. No data found to suggest adverse effect; signal to suggest slight decrease in disease severity in patients on medications.
September 4, 2020:
- Association Between Administration of Systemic Corticosteroids and Mortality Among Critically Ill Patients With COVID-19: A Meta-analysis. 9/2/20. The WHO Rapid Evidence Appraisal for COVID-19 Therapies (REACT) Working Group. JAMA.
This WHO-designed prospective meta-analysis combined data from seven randomized, placebo-controlled trials of corticosteroids in COVID-19 patients with severe disease (with and without mechanical ventilation). All-cause mortality was lower at 28 days in patients treated with corticosteroids, regardless of age, sex or duration of symptoms. Steroid treatment was not associated with increased adverse events. Optimal dose and duration of steroid treatment could not be determined. Of note, trials since June have been modified or terminated early after the RECOVERY trial showed significant benefit from dexamethasone. Numerous tables and graphs elaborate on the complexity of the findings and details.
Other important steroid studies include:- Effect of Hydrocortisone on Mortality and Organ Support in Patients With Severe COVID-19: The REMAP-CAP COVID-19 Corticosteroid Domain Randomized Clinical Trial
- Effect of Hydrocortisone on 21-Day Mortality or Respiratory Support Among Critically Ill Patients With COVID-19: A Randomized Clinical Trial
- Effect of Dexamethasone on Days Alive and Ventilator-Free in Patients With Moderate or Severe Acute Respiratory Distress Syndrome and COVID-19: The CoDEX Randomized Clinical Trial
- Dexamethasone in Hospitalized Patients with Covid-19 — Preliminary Report
- Corticosteroids in COVID-19 ARDS: Evidence and Hope During the Pandemic. 9/2/20. Prescott HC. JAMA.
This succinct, informative editorial reviews the controversy, data and use of corticosteroids for ARDS in the pre-COVID-19 era, then summarizes the best studies and the WHO meta-analysis. “Corticosteroids appear to be associated with benefit among critically ill patients with COVID-19.” The authors also applaud the work and collaboration of researchers conducting these trials in difficult circumstances. - COVID-19-associated hyperinflammation and escalation of patient care: a retrospective longitudinal cohort study. 8/21/20. Manson JJ. Lancet Rheumatol.
A retrospective observational cohort study of 269 consecutive adult inpatients from the UK during March 2020 identified a “hyperinflammatory” subgroup predictive of a considerably higher risk of severe disease or death based upon C-reactive protein >150 mg/ml or a doubling from >50 mg/L w/in 24 hours, or Ferritin levels >1500 μg/L. These simple biomarkers had a predictive hazard ratio of 2.2 (1.6-2.9) for next-day escalation of support or death. 40% of the subgroup died vs. 26% of others. Follow-up was > 28 days or until death. - Effect of Dexamethasone on Days Alive and Ventilator-Free in Patients With Moderate or Severe Acute Respiratory Distress Syndrome and COVID-19: The CoDEX Randomized Clinical Trial. 9/2/2020. Tomazini BM. JAMA.
The CoDex trial measured the effect of iv dexamethasone plus standard care on ventilator free days within 28 days of admission among 300 patients in 41 critical care units in Brazil. A comparison group received standard care only. There was a difference of 2.26 days between groups in favor of dexamethasone (95% CI). - Effect of Hydrocortisone on 21-Day Mortality or Respiratory Support Among Critically Ill Patients With COVID-19: A Randomized Clinical Trial. 9/2/2020. Dequin PF. JAMA.
Low dose hydrocortisone decreased mortality or ongoing need for mechanical ventilation or high flow oxygen when compared to placebo. The study was terminated early and the result between groups was not significant. - Effect of Hydrocortisone on Mortality and Organ Support in Patients With Severe COVID-19: The REMAP-CAP COVID-19 Corticosteroid Domain Randomized Clinical Trial. 9/2/2020. The Writing Committee for the REMAP-CAP Investigators. JAMA.
Among patients with severe COVID-19, intravenous hydrocortisone administered as 7-day fixed dose or given to patients requiring circulatory support only, improved survival and days free of intensive care unit-based respiratory or cardiovascular support within 21 days. Since the trial was stopped early, statistical significance was not achieved but the median adjusted odds ratio for improvement was 1.43 and the probability of superiority 93% in the fixed dose group and 1.22 80% in the shock dependent group. - Humoral Immune Response to SARS-CoV-2 in Iceland. 9/1/20. Gudbjartsson DF. N Engl J Med.
Fifty-six percent of all SARS-CoV-2 infections in Iceland had been diagnosed with quantitative polymerase-chain-reaction (qPCR) assay, 14% had occurred in quarantined persons who had not been tested with qPCR (or who had not received a positive result, if tested), and 30% had occurred in persons outside quarantine and not tested with qPCR. Despite extensive screening by qPCR, a substantial fraction of infections were not detected, which indicates that many infected persons did not have substantial symptoms. But due to the low SARS-CoV-2 antibody seroprevalence, the Icelandic population is vulnerable to a second wave of infection. - Marked factor V activity elevation in severe COVID-19 is associated with venous thromboembolism. 8/24/2020. Stefely JA. Am J Hematol.
This article studies Factor V association with COVID-19 in 102 patients. This is a well-done study and offers possible clinical effects on care and future routes for investigation. The authors found an extraordinary level of factor V elevation in COVID-19 patients which had not been observed in any patient group in the past. A number of other clotting parameters were also analyzed. This patient group consisted primarily of those representing severe cases requiring ventilators. Factor V changes were associated with the wide variety of other clotting parameters and clinical events. This reviewer is not surprised at alterations in factor V levels since this disease is associated with an incredible degree of activation of clotting and related systems. - SARS-CoV-2 another kind of liver aggressor, how does it do that?. 8/29/2020. Lozano-Sepulveda SA. Ann Hepatol.
This is an overview of all the recent findings regarding the molecular biology of the virus and its several modes of assault on liver disease in COVID. Authors conclude the cross-talk cellular protein virus is pivotal for its harmful injury to the liver. Admits the pathogenesis is multifactorial, evolving understanding of pathogenesis. Its natural history of the disease is unestablished. It has an informative cartoon. - SARS-CoV-2 RNA in serum as predictor of severe outcome in COVID-19: a retrospective cohort study. 8/28/2020. Hagman K. Clin Infect Dis.
These authors in this retrospective study have an observation for COVID-RNA in Serum (n= 61, + ve=high viral load e.g. unable to control viral replication) at admission (10th day symptoms) met with an outcome of critical disease or mortality with the hazard ratios of 7.2 and 8.6, respectively for critically ill patients compared to serum PCR negative (n= 106) group. Authors infer -Not detecting COVID-RNA in serum indicated a high chance of uncomplicated recovery. The disease severity was based on clinical profile (age, comorbidities) in this cohort. Noted with statistics age (& other comorbidity), decreases the ability to control viral replication. Detection of COVID in serum likely to be due to the inflammatory response or hematogenous spread of virus possibly more advanced stage of the infection/ inflammation. Other potential antiviral therapies (Remdesivir, convalescent plasma, steroid, IL 6 blockers) may have roles clearing the infection especially serum PCR positive patients to avoid the development of critical disease/death. Both groups had all the available (& variable) treatment (convalescent plasma, steroid, antiviral drugs). The PCR in serum was done 2 different methods in an overlap. - Symptoms of Anxiety, Depression and Peritraumatic Dissociation in Critical Care Clinicians Managing COVID-19 Patients: A Cross-Sectional Study. 8/31/20. Azoulay E. Am J Respir Crit Care Med.
A survey of French ICU healthcare workers, using the Hospital Anxiety and Depression Scale (HADS) and Peritraumatic Dissociative Experience Questionnaire (PDEQ), resulted in a 67% response (n=1058). Most disturbing: 23.7% reported beginning or increasing use of tobacco, alcohol, cannabis, cocaine, or other drugs during the pandemic. Prevalence of anxiety (50%), depression (30%), and peritraumatic dissociation (32%) was highest among nurses and lower among males. Potentially modifiable factors included fear of infection, inability to rest or care for family, difficult emotions, restrictive visitation policies, and witnessing hasty end-of-life decisions. Psychological burden among ICU providers is high during the COVID-19 epidemic. Institutions and individuals should strive to reduce modifiable factors.
September 2, 2020:
- Anakinra in COVID-19: important considerations for clinical trials. 5/21/20. King A. Lancet Rheumatol.
This comment is of interest for clinicians and researchers working with the Interleukin IL-1α and IL-1β inhibitory agent anakinra in COVID-19 patients with evidence of hyperinflammation. The authors review and critique 10 ongoing trials with anakinra and suggest using worsening lymphopenia as a marker of disease progression and severity and increasing C-reactive protein as evidence of worsening inflammation. They also favor subcutaneous administration due to the drug’s short half-life and implore the trial gate keepers to ensure collection of core outcome measures, like ferritin levels for current and future trials. - Respiratory physiology of COVID-19-induced respiratory failure compared to ARDS of other etiologies. 8/28/20. Grieco DL. Crit Care.
This article provides a detailed comparison of the respiratory mechanics of 30 COVID-19 ARDS patients measured within 24 hours of initial intubation with 30 non-COVID matching ARDS patients based on PaO2/FiO2, FiO2, PEEP, and tidal volume. The average compliance and ventilatory ratio were slightly higher in COVID-19 patients. Inter-individual variability of compliance was similar in both groups. In COVID-19 patients, PaO2/FiO2 was linearly correlated with respiratory system compliance. High PEEP improved PaO2/FiO2 in both cohorts, but more remarkably in COVID-19 patients. Recruitability was not different between cohorts. The authors conclude that overall the respiratory mechanics were similar in the two groups but were marked by prominent intra-group variability in both. - Viral dynamics and immune correlates of COVID-19 disease severity. 8/28/20. Young BE. Clin Infect Dis.
One hundred COVID-19 patients from Singapore underwent prospective study of infectivity and immune response on days 1, 3, 7,14, 21 and 28 after enrollment. No positive viral cultures were found in respiratory samples (n=21) obtained more than 14 days after symptom onset and all positive viral cultures occurred in patients with PCR cycle threshold values <30. Disease severity was associated with earlier seroconversion, higher peak IgM and IgG levels, and higher levels of inflammatory markers, but not duration of viral shedding by PCR. Results have implications for duration of isolation/quarantine and from whom to potentially obtain convalescent plasma.
August 31, 2020:
- A meta-analysis of the incidence of venous thromboembolic events and impact of anticoagulation on mortality in patients with COVID-19. 8/9/20. Lu YF. Int J Infect Dis.
This well-written meta-analysis describes DVT and COVID-19 and the effect of anticoagulation on mortality. It raises good points for discussion. - Cardiac Injury Patterns and Inpatient Outcomes Among Patients Admitted With COVID-19. 7/23/20. Raad M. Am J Cardiol.
This is a retrospective analysis of 1020 patients with confirmed COVID-19 disease of which 390 (38%) had cardiac injury on presentation diagnosed by hs-cTnI levels >99% tile; primary endpoint was mortality and secondary were intensive care requirement and length of stay. Patients were older (median 70), higher cardiac co-morbidities (hypertension, diabetes) and all had BMI >30. Higher troponin levels associated with mortality and ICU requirements including mechanical ventilation. Results confirm previous studies associating cardiac involvement due to COVID-19 with increasing severity associated with cardiac related co-morbidities. - Haemodynamic Monitoring and Management in COVID-19 Intensive Care Patients: An International Survey. 8/9/20. Michard F. Anaesth Crit Care Pain Med.
This article describes an interesting and unique data set resulting from a survey of 1000 anesthesiologists and intensivists on the assessment of hemodynamics from around the globe. It documents the methods for hemodynamic assessment of critically ill patients and compares practice patterns in various parts of the world. - How Do Presenting Symptoms and Outcomes Differ by Race/Ethnicity Among Hospitalized Patients with COVID-19 Infection? Experience in Massachusetts. 8/22/20. McCarty TR. Clin Infect Dis.
Association of Race With Mortality Among Patients Hospitalized With Coronavirus Disease 2019 (COVID-19) at 92 US Hospitals. 8/18/20. Yehia BR. JAMA Netw Open.
Two studies are combined here, a retrospective analysis of nine Massachusetts hospitals including all consecutive adult patients hospitalized with laboratory-confirmed COVID-19; and another of patients enrolled in the Ascension hospitals, in a cohort of 92 hospitals across 12 states. Both groups of authors found no association between race/ethnicity and clinically relevant outcomes of hospitalization, including mortality, among patients hospitalized with COVID-19. As has been seen in other research, older age and male sex were significantly associated with risk of death. - Immune response to SARS-CoV-2 in health care workers following a COVID-19 outbreak: A prospective longitudinal study. 8/11/2020. Fill Malfertheiner S. J Clin Virol.
To continue the operation of German perinatology unit during the pandemic, the authors decided to study (complicated & sophisticated) longitudinally the immune response of 166 (RT PCR + Ve n= 31) health care workers for 8-12 weeks. The authors concluded that the immune response after a COVID-19 outbreak increases significantly over time but still approximately 22% of COVID-19 patients did not have a measurable serologic immune response within 60 days after symptoms. Additionally summarize that exposed co-workers did not develop any relevant IgG antibody levels over time. Meaning no silent seroconversion in HCW from diseased coworkers. IgA is not an adequate marker for long-term immunity. The HCW in the facility can be protected by the necessary measures that are taken fast and furiously with protective measures as neither immunity after infection nor herd immunity are reliable. - Management of Thrombotic Complications in COVID-19: An Update. 8/16/20. Hajra A. Drugs.
This article encompasses treatment of DVT with COVID-19, and is a good update compared to prior comprehensive summaries. - Microwave- and Heat-Based Decontamination of N95 Filtering Facepiece Respirators: A Systematic Review. 8/24/2020. Gertsman S. J Hosp Infect.
This systematic review looked at data from 13 (2007-2020) reports involving heat or microwave-based decontamination of N95 respirators. Both 60-90°C heat and microwave methods were found generally effective to deactivate viral pathogens and maintain respirator fit and function. Higher heat and autoclave methods sometimes caused significant degradation. Firm conclusions difficult to reach due to heterogeneity of mask models, methods, and assessments as well as lack of real-world fit testing. No advice on number of cycles is reported. Monitoring of durability is strongly advised. - Role for Anti-Cytokine Therapies in Severe Coronavirus Disease 2019. 8/25/20. Buckley LF. Crit Care Explor.
This is an excellent detailed review summarizing existing knowledge of the immune response (cytokine injuries) to coronavirus infection and highlights the current and potential future roles of therapeutic strategies to combat the hyper-inflammatory response of patients with COVID-19. Here, details regarding immunopathogenesis, pharmacodynamics, pharmacokinetics with illustrations are provided for available anti-cytokines pertaining to their success and failure in 3 groups (IL1, IL6 and other cytokine modulators). The authors conclude by advising to look for approximately a dozen future clinical trials to answer questions regarding the dose, timing, biomarkers and other issues of anti-cytokines. Both IL1 and IL6 cytokine blockers have a role in the first wave of inflammation (< 7 days of symptoms), while IL1 blockers are slightly superior having no black box warning for secondary infection as do IL6 and TNF blockers. - Sex differences in immune responses that underlie COVID-19 disease outcomes. 8/26/20. Takahashi T. Nature.
Preliminary data show different immune capabilities and responses for males and females, with implications for disease prevention and treatment strategies. Viral loads, antibody levels, plasma cytokines/chemokines, and blood cell phenotypes were measured in 98 COVID-19 inpatients and 43 healthy controls. Forty-eight patients had longitudinal analysis. Multiple pro-inflammatory immune chemokine and cytokine levels were higher in males, while females demonstrated a more robust baseline T-cell response. T-cell response was negatively correlated with age in males only. Disease progression was inversely associated with T-cell response in males and positively associated with innate immune cytokine levels in females. - Subcutaneous Enoxaparin Safely Facilitates Bedside Sustained Low-Efficiency Hemodialysis in Hypercoagulopathic Coronavirus Disease 2019 Patients-A Proof-of-Principle Trial. 7/23/20. Neumann-Haefelin E. Crit Care Explor.
Faced with recurrent filter clotting and incomplete dialysis in hypercoagulable COVID-19 patients needing renal replacement therapy, these authors changed therapeutic anticoagulation from unfractionated heparin to low molecular weight heparin. In their retrospective study of 3 patients, LMWH markedly increased successful completion of RRT. Their protocol reduces the risk of discarding important resources, filter and blood and at the same time provides adequate dialysis quality. - Transthoracic Echocardiography in Prone Patients With Acute Respiratory Distress Syndrome: A Feasibility Study. 8/25/20. Gibson LE. Crit Care Explor.
Gibson et al. describe the technique, views and utility of performing bedside transthoracic cardiac ultrasound exams on 27 prone, intubated COVID-19 patients in Boston. They found the views obtained prone were sometimes improved over supine images, allowing avoidance of TEE. There are excellent images, videos, and tables. - Treatments Considered for COVID-19. 8/27/2020. The Medical Letter.
This is an exhaustive yet easy to use summary of current COVID-19 therapeutics as of late August.
August 26, 2020:
- A cross-sectional study of immune seroconversion to SARS-CoV-2 in frontline maternity health professionals. 8/10/20. Bampoe S. Anaesthesia.
Two hundred presumably COVID-19-free OB anesthetists, midwives and obstetricians in two tertiary London hospitals were tested for IgG to SARS-CoV-19. Fourteen percent were seropositive, most with no or minimal symptoms in retrospect. The only significant symptom was anosmia. This seroconversion rate is similar to that in the general population in London. In an effort to limit the spread of COVID-19 by infected healthcare workers, the authors suggested regular testing for staff, and isolation for those who develop anosmia or test positive. - Angiotensin Converting Enzyme Inhibitor and Angiotensin II Receptor Blocker Use Among Outpatients Diagnosed With COVID-19. 7/11/20. Bae DJ. Am J Cardiol.
This is a single center retrospective study comparing patients diagnosed with COVID-19 taking ACE/ARB medications versus not taking these medications. Use of ACE/ARB medications was not associated with risk of hospital admission or, if admitted, no differences in all cause mortality, ICU stay, mechanical ventilation requirements or inotrope use. This article confirms prior recommendations to continue use of ACE/ARB medications in COVID-19 patients. - Association Between Youth Smoking, Electronic Cigarette Use, and Coronavirus Disease 2019. 8/11/20. Gaiha S. J Adolescent Health.
This was an online survey conducted of 4,351 adolescents and young adults, aged 13-24 years, from 50 states, DC, and 3 US territories. Users (ever or long-term) of e-cigarettes/tobacco cigarettes were at a higher risk of getting COVID-19 and dual users are even more prone to contract COVID-19. Better screening and education may be indicated. - Clinical Course and Molecular Viral Shedding Among Asymptomatic and Symptomatic Patients With SARS-CoV-2 Infection in a Community Treatment Center in the Republic of Korea. 8/6/20. Lee S. JAMA Intern Med.
Though patients may not be symptomatic, their viral load may be similar to symptomatic patients. Here, 80.9% of patients with SARS-CoV-2 who were asymptomatic at the time of detection of a positive RT-PCR remained asymptomatic during a median of 24 days from diagnosis, and the cycle threshold values in asymptomatic patients were similar to those in symptomatic patients. - Epidemiology of invasive pulmonary aspergillosis among COVID-19 intubated patients: a prospective study. 7/28/20. Bartoletti M. Clin Infect Dis.
This prospective multicenter trial evaluated 108 mechanically ventilated COVID-19 pneumonia patients for pulmonary aspergillosis by clinical features, bronchoalveolar lavage for fungal culture and galactomannan assay, and serum galactomannan assay. Probable “coronavirus-associated pulmonary aspergillosis” (CAPA) was diagnosed in 28%. “Putative invasive pulmonary aspergillosis” (PIPA) was diagnosed in 63% of the CAPA patients. Kaplan-Meier curves showed a significantly higher 30-day mortality rate among patients with either CAPA (44% vs 19% in non-CAPA patients) or PIPA (74% vs 26% in non-PIPA patients). Patients treated for aspergillosis with voriconazole showed a trend towards improved mortality. - The challenge of managing COVID-19 associated pulmonary aspergillosis. 8/18/20. Brüggemann RJ. Clin Infect Dis.
This excellent editorial can serve as a good primer on current approaches to diagnosing clinically significant pulmonary aspergillosis in the general patient population and clarifies some of the important issues specific to diagnosing and treating pulmonary aspergillosis in COVID-19 patients. - What are the sources of exposure in healthcare personnel with coronavirus disease 2019 infection? 8/11/20. Zabarsky TF. Am J Infect Control.
In an analysis at the Cleveland VA Medical Center, 25% of healthcare personnel testing positive for SARS-CoV-2 had a higher-risk exposure at work and an additional 14% of infected personnel reported higher-risk exposures to family members or other infected individuals in the community. The issue was that in certain patients’ rooms where COVID-19 wasn’t suspected, they actually had the disease and nurses were exposed. Then, out in the community, not all wore masks. No cases occurred in personnel working on COVID-19 wards.
August 25, 2020:
- Clinical Outcomes Associated with Methylprednisolone in Mechanically Ventilated Patients with COVID-19. 8/9/20. Nelson BC. Clin Infect Dis.
In this study, methylprednisolone (MP) increased ventilator-free days. In contrast, a randomized controlled study with MP failed to lower mortality while a dexamethasone study demonstrated lower mortality. Study design, varying treatment modalities, timing and co-morbidity might explain the difference in outcomes. - Compliance Phenotypes in Early ARDS Before the COVID-19 Pandemic. 8/17/2020. Panwar R. Am J Respir Crit Care Med.
This study sought to look for the “L” type (preserved lung compliance) phenotype of ARDS in pre-COVID-19 intubated ARDS patients. Data collected prospectively before the COVID-19 pandemic from the large international LUNG-SAFE and ESICM Trials groups revealed a continuum of respiratory system compliance in early ARDS, with one in eight patients fitting the “L” type phenotype. This suggests that preserved lung compliance is not unique to COVID-19 ARDS. - COVID-19 and global health: Influences and implications for education and training support in low- and middle-income countries. 8/12/20. Cooper MG. Anaesth Intensive Care.
Cooper et al present an editorial from Australia and the South Pacific reviewing the pandemic challenges faced by low- and middle-income countries (LMIC). Though COVID-19 numbers are surprisingly low in many LMIC countries, surges are expected. If this happens, the lack of ICU capability, the vulnerability of healthcare workers with limited PPE, the restriction of healthcare worker training, and even lack of oxygen will likely cause major problems, from crumbling of already fragile healthcare systems, to surging poverty and a worsening supply of healthcare workers. - ECMO for severe ARDS associated with COVID-19: now we know we can, but should we? 8/13/20. Shekar K. Lancet Respir Med.
This is a well-written editorial on outcomes and resource use for ECMO treatment of severe COVID-19 ARDS referring to a report of 83 patients treated with ECMO with an estimated 31% probability of death at 60 days similar to that seen in studies of ECMO for severe ARDS outside the pandemic. However, the editorial notes that, 24% of patients were still in the ICU on day 60, and that the median length of ECMO support (20 days) and ICU length of stay (36 days) was very high. The question is posed as to the balance of outcomes and the very costly resources (human and financial) required for long duration ECMO. - Extracorporeal membrane oxygenation for severe acute respiratory distress syndrome associated with COVID-19: a retrospective cohort study. 8/13/2020. Schmidt M. Lancet Respir Med.
An outcome report for 87 patients treated with ECMO noting an estimated 31% probability of death at 60 days, similar to that seen in studies of ECMO for severe ARDS outside the pandemic. - Highly sensitive quantification of plasma SARS-CoV-2 RNA sheds light on its potential clinical value. 8/17/20. Veyer D. Clin Infect Dis.
Testing plasma for SARS-CoV-2 RNAaemia with an ultrasensitive droplet-based technique is now possible. It provides more quantitative data than standard RT-PCR tests (free of potential influence by viral inhibitors). This preliminary study of 58 COVID-19 patients and 12 healthy controls showed correlation between both test positivity and RNAaemia level with disease severity. Whether or not positive serum tests detect viable virus is unknown. If validated in larger studies, this tool may provide insights regarding possible viral seeding of organs remote from initial respiratory strongholds, elucidate disease mechanisms, and help identify those at increased risk for poor outcomes. - Inactivation of SARS-CoV-2 and Diverse RNA and DNA Viruses on 3D Printed Surgical Mask Materials. 8/12/20. Welch JL. Infect Control Hosp Epidemiol.
In a step toward solutions for personal protective equipment (PPE) shortages, investigators tested viral disinfection methods on multiple 3D-printed materials. Complete inactivation of multiple viruses including SARS-CoV-2 was demonstrated with a single application of 10% bleach, quaternary ammonium sanitizer, 3% hydrogen peroxide or 70% isopropyl alcohol and exposure to heat (50°C, and 70°C). 70°C dry heat for 30 minutes completely inactivated all viruses tested. 70% isopropyl alcohol reduced viral titers significantly less well following a single application. Materials remained intact after 100 exposures. - Increased mortality in patients with severe SARS-CoV-2 infection admitted within seven days of disease onset. 8/11/20. Azoulay E. Intensive Care Med.
This is a multicenter, retrospective study of 379 COVID-19 patients admitted to four Paris ICUs between 02/20 and 04/24 analyzing mortality and disease severity. The study found that ICU admission within one week of symptom onset was associated with increased mortality due to overall disease severity and multi-organ failure rather than primary respiratory failure. The article provides stimulus for further research to follow progression of disease with opportunity to target therapy depending on disease stage. - Resilience strategies to manage psychological distress among healthcare workers during the COVID‐19 pandemic: a narrative review. 6/13/20. Heath C. Anaesthesia.
This article, dealing with the well-being of healthcare workers in this or future pandemics, has well-proven suggestions to adopt at the self and organizational level. The authors have a holistic approach to reduce the morbidity of high-stressed healthcare workers. Psychological, emotional stress may result in: PTSD, substance abuse, isolation, poor judgments, separation, inefficiency of work, absenteeism, premature burnout, depression, and anxiety. The authors’ remedies include increase in emotional intelligence, resilience, altruism, and adaptive coping mechanism. Emphasis on self-care, sleep, exercise, friends/ family support, mindfulness, a role of organizational justice in debriefing, town hall meetings, training modules furthering resilience, and “battle buddies” (based on the US Army peer-support system). The article has support from several studies to prove their recommendations and its positive results. - Timing of Intubation and Mortality Among Critically Ill Coronavirus Disease 2019 Patients: A Single-Center Cohort Study. 8/14/20. Hernandez-Romieu AC. Crit Care Med.
Results from a cohort analysis to determine if time to intubation in patients receiving supplemental oxygen therapy including high-flow nasal cannula (HFNC) differed from that of patients intubated earlier in the disease course. Despite finding that of those patients receiving HFNC who subsequently required mechanical ventilation (MVA) (71.6%) showed higher initial Sequential Organ Failure Assessment scores; time to intubation had no discernible mortality impact. - What every intensivist should know about COVID-19 associated acute kidney injury. 8/11/20. Ostermann M. J Crit Care.
Acute kidney injury (AKI) is a serious complication in the ICU (incidence < +/- 30%) with COVID-19 patients. The authors explore various etiologies: hypovolemia, hemodynamic instability, inflammation (direct viral invasion, microvascular thrombosis, and dysregulated renin-angiotensin-aldosterone system (RAAS) and of ACE II, iatrogenicity as well). There are no specific therapies for prevention or management of AKI guidelines. Detailed discussion of alternatives to renal replacement therapy (RRT) and other supportive measures are described. An overwhelming need for RRT practice is likely to be determined by the ground reality. A close collaboration between critical care medicine and renal services is essential when resources may be scarce.
August 19, 2020:
- A physiological approach to understand the role of respiratory effort in the progression of lung injury in SARS-CoV-2 infection. 8/10/20. Cruces P. Crit Care.
A thorough, well-written review of the physiology of patient-induced lung injury and of ventilator-induced lung injury adding information from the authors’ detailed CT scan profiles of lung injury in animal models. The article concludes with a balanced discussion of when to support Covid-19 pneumonia patients with non-invasive measures such as high flow nasal cannula versus when to intubate and support with mechanical ventilation. While no new approaches are provided, their recommendations support a complete evaluation of the patient’s condition and show clear consideration for the consequences of patient-induced lung injury. - Association Between Anxiety and New Organ Failure, Independently of Critical Illness Severity and Respiratory Status: A Prospective Multicentric Cohort Study. 7/30/20. Mazeraud A. Crit Care Med.
Interesting, multi-center prospective study evaluating patient’s admission anxiety level on new organ system failure within seven days following ICU admission. While not directly related to COVID-19 (or any specific admission diagnosis), patients identified with moderate to severe anxiety (State anxiety-assessed using state component of State-Trait Anxiety Inventory State) associated with disease severity (Simplified Acute Physiology Score II and Sequential Organ Failure Assessment) associated with increased risk for further deterioration when compared to lower stress comparators. Interesting with obvious implications for current pandemic given long prodrome with variable symptomatology and outcome increasing general anxiety in population with some estimates indicating a recent reported 25% incidence of suicidal ideation in younger age groups. - Convalescent plasma for COVID-19. 8/8/20. Mucha SR. Cleve Clin J Med.
While convalescent plasma has yet to be proven effective, it has generated great interest as a possible COVID-19 therapy and clinical trials are underway. For those interested in a well-written review of the questions and potential risks that must be taken into consideration, this report is a worthwhile read. Potential downsides include TACO, TRALI, antibody dependent enhancement of infection and attenuated immune response. Current limitations include obstacles to effective testing of donor neutralizing antibody levels. This topic is at the center of the current controversy surrounding a potential FDA emergency use authorization for convalescent plasma, (now on hold). - Delirium and encephalopathy in severe COVID-19: a cohort analysis of ICU patients. 8/8/20. Helms J. Crit Care.
Following up on the concept that neurotropism of the SARS-CoV-2 virus has been confirmed, French investigators focused on the neurological status of 140 consecutive patients with COVID-19 linked ARDS (mean age 62, 71% male) to determine the incidence of delirium and abnormal neurological exams. 84% developed delirium and of those, 69% presented with agitation and 63% had long-tract signs. Of 28 patients who underwent lumbar puncture and MRI, 65% had perfusion abnormalities and 61% had signs of a disturbed blood brain barrier, 64% showed inflammatory signs in CSF and one was PCR positive for SARS-CoV-2 in CSF. Delirium associated with ARDS and COVID-19 is a distinct entity caused by the corona virus which prolongs and complicates recovery, both short term and possibly in the long term as well. - Extracorporeal membrane oxygenation for refractory COVID-19 acute respiratory distress syndrome. 7/31/20. Le Breton C. J Crit Care.
A brief single center report stating that 11 of 13 patients treated with ECMO were successfully weaned from ECMO (medium treatment of 13 days) and eventually from mechanical ventilation (median treatment 29 days). The authors support ECMO use in carefully selected cases. - Infection Prevention Precautions for Routine Anesthesia Care During the SARS-CoV-2 Pandemic. 8/3/20. Bowdle A. Anesth & Analg.
Authors promote precautions that are practical, affordable, and efficient to adjust routine anesthesia care to the current and near-future environment. Consideration for asymptomatic and pre-symptomatic SARS-CoV-2 infection, and the potential for false-negative tests inform recommendations to reduce the risk of transmission via anesthesia care behaviors. Universal N95 or higher respiratory protection is proposed for anesthesia providers with consideration given to whether the entire surgical team should use equivalent respiratory protection. Tables provide a useful summary of PPE, hand hygiene and other recommendations. - Late Onset Infectious Complications and Safety of Tocilizumab in the Management of COVID-19. 8/14/20. Pettit NN. J Med Virol.
Tocilizumab while previously showing some positive results in treating COVID-19, in this controlled study demonstrated higher complication rates, especially infectious, and death. - Prominent coagulation disorder is closely related to inflammatory response and could be as a prognostic indicator for ICU patients with COVID-19. 8/8/20. Liu Y. J Thromb Thrombolysis.
Interesting discussion highlighting interrelationship between inflammatory and coagulation systems; suggests coagulation abnormalities (PT, D-Dimer, FDP and AT III) can predict deterioration and mortality; also notes the neutrophil/lymphocyte ratio is a potential inflammatory marker in disease. Recognizes importance of prophylactic thromboprophylaxis and accurate timing of systemic anticoagulation. - Unspecific post-mortem findings despite multiorgan viral spread in COVID-19 patients. 8/12/20. Remmelink M. Crit Care.
The authors found in this study of 17 patients, a great heterogeneity of COVID-19-associated organ injury and the remarkable absence of any specific viral lesions, even when RT-PCR identified the presence of the virus in many organs. Pulmonary findings revealed early-stage diffuse alveolar damage 15/17; microthrombi in small lung arteries in 11 patients and no evidence of myocarditis, hepatitis, or encephalitis. Onset of symptoms and death ranged from 2 to 40 days.
August 17, 2020:
- Characteristics and outcomes of pregnant women admitted to hospital with confirmed SARS-CoV-2 infection in UK. 6/8/20. Knight M. BMJ.
At all 194 obstetric units in the United Kingdom, 4.9 per 1000 pregnant women (n=427) were hospitalized with confirmed SARS-CoV-2 infection between March 1, 2020 and April 14, 2020. Sixty-nine percent were overweight or obese. Fifty-eight percent had symptom onset >32 weeks gestational age. By study end, 62% (n=266) had completed pregnancy with 259 live births, 3 still births and 4 lost pregnancies. Of those, 74% (n=196) were term births,16% (n=42) had C/section “due to COVID-19,” and 44% (n=114) had C/section for other reasons. Among all hospitalized, 10% needed ICU, 1% were placed on ECMO, and 1% died. Five percent of 265 infants were RNA+ for SARS-CoV-2. Results resemble USA reports. - Role of children in household transmission of COVID-19. 8/7/2020. Kim J. BMJ.
Contact Tracing during Coronavirus Disease Outbreak, South Korea, 2020. 7/16/2020. Park YJ. Korea Centers for Disease Control and Prevention.
These two articles from the South Korean Centers for Disease Control and Prevention describe their thorough contact tracing program and results at the beginning of the pandemic, when quarantining was compulsory and rigorous in South Korea. The details of the tracing, follow-up and protocol are informative. Across all ages of index patients, contact positivity was 11.8% (in household contacts) and 1.9% (in non-household contacts). For index patients 1 – 18 years old, the contact positivity rate was 0.5%. This information has been noted while trying to reopen schools, though the public health standards in schools are different than during lockdown in South Korea. - COVID-19: pharmacology and kinetics of viral clearance. 8/8/20. Farina N. Pharmacol Res.
In addition to critically reviewing the results of currently available therapeutic options, investigators examined viral clearance dynamics in a cohort of 1000+ patients enrolled in a COVID-19 hydroxy-chloroquine and lopinavir/ritonavir research protocol at a single center in Milan. Viral clearance was assessed as time to negative RT-PCR as well as determining the proportion of patients with a negative test within 14 and 28 days. Significantly, persistence of the virus did not identify patients with higher mortality risk. - COVID-19 and Dexamethasone: A Potential Strategy to Avoid Steroid-Related Strongyloides Hyperinfection. 7/30/20. Stauffer WM. JAMA.
Dexamethasone is recommended for critically ill COVID-19 patients. One of its uncommon preventable complications is strongyloides hyperinfection caused by a nematode (roundworm). Seroprevalence of strongyloides ranges from 10-15% among migrants from less developed countries. The infection can last a lifetime. Hyperinfection appears to be independent of dose or duration of steroid. Its possibility should be considered if the patient deteriorates acutely. For outpatients, the authors recommend screening for strongyloides and treating with ivermectin if positive. For inpatients, they recommend presumptive treatment with ivermectin for patients not previously tested or treated for strongyloides. - Impact of the Coronavirus Infection in Pregnancy: A Preliminary Study of 141 Patients. 7/7/20. Nayak AH. J Obstet Gynaecol India.
They studied 141 pregnant COVID positive women and 836 pregnant controls in Mumbai, India from April 1, 2020 to May 15, 2020. COVID-19 did not have a major adverse effect on maternal or newborn outcomes. Mortality was 2% and morbidity was low among COVID-positive mothers. Out of a total of 131 babies tested, only 3 tested positive on first swab and all tested negative on day 5. Vertical transmission of COVID-19 infection from mother to newborn was rare. This study reports fewer adverse outcomes than some others. - Systematic SARS-CoV-2 screening at hospital admission in children: a French prospective multicenter study. 7/25/20. Poline J. Clin Infect Dis.
In a small French study of consecutive children admitted to the hospital, 45% were not able to be diagnosed with COVID-19 on symptoms alone. A pre-existing underlying condition did not alter the rate of infection. This study demonstrates that routine symptom screening for COVID-19 frequently fails. - Tracking Changes in SARS-CoV-2 Spike: Evidence that D614G Increases Infectivity of the COVID-19 Virus. 7/2/20. Korber B. Cell.
Herd immunity and vaccines for SARS-CoV-2 are likely to be effective due to low mutation rates. D614 was the original spike protein form. G614 is now dominant, although there are other mutations. G614 is ~10x more infectious and leads to higher viral loads but does not cause more severe clinical disease. It is being targeted for the development of vaccines and therapeutics.
August 14, 2020:
- Cerebrovascular Complications of COVID-19. 8/8/20. Katz JM. Stroke.
Retrospective case review focusing on imaging confirmed stroke incidence among COVID-19 inpatients treated in a largely metropolitan health care system. 86 stroke patients were identified and compared to 499 stroke patients admitted a year earlier. COVID-19 patients were significantly more likely to have a stroke while hospitalized (48% vs 5%). Additional important findings among the COVID-19 group includes a predominance of ischemic stroke and a high frequency (67%) of non-focal neurologic presentations and a higher incidence among racial minorities.
In-hospital stroke among COVID-19 patients is a strong independent risk factor and deserves a high grade of suspicion when patients develop neurologic symptoms. - Multisystem Inflammatory Syndrome in Children (MIS-C) Associated with SARS-CoV-2: A Systematic Review. 8/4/20. Abrams JY. J Pediatr.
This article is a comprehensive description of multisystem inflammatory syndrome in children (MIS-C) authored by Centers for Disease Control scientists. - SARS-CoV-2 viral load in the upper respiratory tract of children and adults with early acute COVID-19. 8/6/20. Baggio S. Clin Infect Dis.
This prospective cohort study from Switzerland compared the viral load in patients of all ages during the first 5 days of COVID-19 symptoms. Viral loads as measured by cycle thresholds of RT-PCR testing were similar across all age groups (0-82 years old). This study of viral load in symptomatic patients helps clarify confusing results from other studies and may be especially pertinent as schools try to reopen. - The COVID-19 Vaccine Race: Challenges and Opportunities in Vaccine Formulation. 8/5/20. Wang J. AAPS PharmSciTech.
This article is an in-depth review of vaccine development and delivery strategies, particularly as they apply to SARS-CoV-2. The proper choice of the type of vaccine, carrier or vector, adjuvant, excipients (other ingredients), dosage form, and route of administration can directly impact not only the immune responses and efficacy against COVID-19, but also the logistics of manufacturing, storing, distributing the vaccine and mass vaccination. The 13 vaccines under development (as of May 29, 2020) are nicely compared. The tables and graphics are excellent.
August 12, 2020:
- Case Rates, Treatment Approaches, and Outcomes in Acute Myocardial Infarction During the Coronavirus Disease 2019 Pandemic. 8/7/20. JAMA Cardiol.
Using discharge coding of >15,000 acute MI hospitalizations over 17 months from a multi-state US health system, a significant decrease in observed vs. expected numbers during the early COVID-19 period, March-May 2020, was observed in all regions. NSTEMI patients disproportionately decreased and hospital cardiac death rates increased, particularly in STEMI patients. Trends largely normalized by study end, May 10, 2020. These data suggest that patients avoided presenting to hospital with possible AMI during the early COVID-19 period, potentially forfeiting the benefit of early reperfusion in some cases. - COVID-19 interstitial pneumonia: monitoring the clinical course in survivors. 8/3/20. Raghu G. Lancet Respir Med.
This may appeal more to research physicians and not frontline workers. This “Comment” letter from two American pulmonary physicians identifies a need to follow COVID-19 survivors to better understand the natural course of the pulmonary disease after hospitalization and discover the influence of treatments. They outline an extremely thorough series of medical visits and tests to accomplish this goal. - Evaluation of Coronavirus Disease 2019 Severity Using Urine Biomarkers. 8/9/2020. Katagiri D. Crit Care Explor.
A urinary, 58 pts study testing for severity and progression of COVID-19. Levels of β2-microglobulin, liver-type fatty acid-binding protein (L-FABP) were correlated to severity and progression of active infection. Not accurate in presence of renal disease nor does the paper describe specificity to COVID-19. - International variation in the management of severe COVID-19 patients. 8/5/2020. Azoulay E. Crit Care.
As the title suggests, there are international variations in the treatment of COVID-19 patients as evidenced from a survey sent to 1132 multinational ICU physicians from the ESICM regarding management of a case vignette. Responses varied across regions and may reveal resource constraints, individual bias, lack of standardization and local preference.
August 10, 2020:
- Characterization of the Inflammatory Response to Severe COVID-19 Illness. 6/25/2020. McElvaney OJ. ATS.
This article offers a detailed measurement of inflammatory mediators in 20 severely ill patients compared with a group of moderately ill patients and a group of normal controls. It’s proposed that similar characterisations and treatment trials might someday allow for a tailor made treatment regimen of immune modulators to be given to each patient optimizing their recovery. The accompanying editorial highlights the finding in the original study that alpha-1-antitrypsin (AAF), which has an anti-inflammatory effect, is reduced in patients with severe Covid-19 pneumonia, and a trial of AAF supplementation may be warranted. - Determination of brain death/death by neurologic criteria: the World Brain Death Project. 8/30/20. Sung GY. JAMA.
Published by a panel of 40+ international experts, this is a thorough and comprehensive guideline aiming to establish worldwide recognized brain death criteria and testing methods. - Feasibility and clinical impact of out-of-ICU non-invasive respiratory support in patients with COVID-19 related pneumonia. 8/3/20. Franco C. Eur Respir J.
This is a retrospective analysis of 670 patients admitted to nine hospitals in northern Italy between March 1 and May 10 with documented COVID-19 infection and whom required oxygen support beyond nasal oxygen treated with non-invasive support methods (HFNC, CPAP, NIV) in specialized respiratory but non-ICU settings. Units were staffed (N/P ratios ranged from 1:6-1:2) and all units were well ventilated with natural air flow. Patients were spaced more than 5 feet apart. All staff engaged in care wore appropriate PPE. Outcomes were effectiveness of treatment (28 day unadjusted mortality of 26.9%) and HCW infection (11.4%; 3.3% ill). Adjusting for confounders, there was no difference between HFNC, CPAP and NIV. Discussion includes advanced directive understanding/use in Italy and value of pre-allocated respiratory wards. - High Respiratory Drive and Excessive Respiratory Efforts Predict Relapse of Respiratory Failure in Critically Ill Patients with COVID-19. 8/5/20. Esnault P. Am J Respir Crit Care Med.
This is a retrospective study of 28 patients with moderate to severe ARDS evaluating the use of P0.1 (airway occlusion pressure decrease at 100 msecs after expiratory flow is zero) and ΔPocc, (the maximum negative airway pressure decrease occurring during a full cycle end-expiratory occlusion) to predict failure of weaning from the ventilator. They propose using P0.1 as an automatically generated measure on most current ventilators. A P0.1 of ≥ 4cmH2O predicts failure to wean with a sensitivity of 89% and a specificity of 74%. The ΔPocc was less discriminating than P0.1. - Therapeutic plasma exchange in adult critically ill patients with life-threatening SARS-CoV-2 disease: A pilot study. 7/31/20. Faqihi F. J Crit Care.
This article reports preliminary data on total plasma exchange as rescue therapy for 10 consecutive eligible adult COVID-19 ICU patients. (Technique using Spectra Optia™ Apheresis System w/ Depuro D200 Adsorption Cartridge and volume replacement w/ 5% albumin or fresh frozen plasma if PT>37 sec.) All patients were mechanically ventilated and had life-threatening illness and cytokine release syndrome (average PaO2/FiO2 ratio 110, SOFA 11, APACHE II 22.5). After 5-7 treatments P/F >250 in all and vasopressors weaned. One on ECMO, 2 had PE, and there was 1 sudden death during ventilator weaning. Nine patients were discharged from hospital. No reported adverse effects. Confounding factors include steroid and other concurrent treatments.
(Note: this is not convalescent plasma treatment.) - Editorial: Attenuating hyperinflammation in COVID-19: A change in paradigm? 7/23/20. Molnar Z. J Crit Care.
This editorial accompanying Faqihi’s report of total plasma exchange as rescue therapy for life-threatening COVID-19 presents an interesting discussion of the history of our understanding of host-based detrimental “dysregulated immune responses” including “cytokine storm,” along with potential blood purification therapies. The good news is that multiple trials in this domain are registered on ClinicalTrials.gov.
August 7, 2020:
- Post-discharge venous thromboembolism following hospital admission with COVID-19. 8/3/20. Roberts LN. Blood.
These authors identified 1,877 patients with COVID-19 discharged from the hospital, and noted that there were nine episodes of Hospital Associated Venous Thromboembolism (HA-VTE) diagnosed within 42 days compared with 2019 hospital discharge data. The authors calculated an odds ratio of 1.6 compared to historically “similar” groups of patients. They concluded that hospitalization of patients with COVID-19 does not appear to increase the risk of post-discharge HA-VTE compared to hospitalization with other acute medical illnesses. Their data suggests empiric post-discharge thromboprophylaxis is not necessary, thereby supporting the ACCP recommendations to not offer post-discharge thromboprophylaxis. - Reopening Primary Schools during the Pandemic. 7/29/20. Levinson M. N Engl J Med.
This is a narrative summary and commentary on the literature and debate around reopening primary schools in the US, written by educators and medical epidemiologists. Primary schools in many other countries have re-opened successfully for in-person classes, but that success hinged on low community transmission rates, and extensive testing and surveillance. The authors believe that there is time in the US to achieve successful reopening in some areas if resources and effort are increased. The argument is made that primary schools are essential services, and “whether (or how) to reopen primary schools is not just a scientific and technocratic question. It is also an emotional and moral one.” - Reprocessing filtering facepiece respirators in primary care using medical autoclave: prospective, bench-to-bedside, single-centre study. 8/4/20. Harskamp RE. BMJ Open.
Dutch investigators studied standard autoclave machines for decontamination of FFP2 and FFP3 respirators. They found that one model of FFP2 (the closest European Standard to US N95 respirators) tolerated up to 3 decontamination cycles at 121°C x 17 min. without significant change in filtration, resistance, or fit. Others, including the tested FFP3 model (higher filtration), did not. Referenced published studies support efficacy of this temperature to kill SARS-CoV-2. This study corroborates great variation between mask models observed in other studies and the critical importance of careful fit testing with each donning when considering decontamination and reuse of filtering facepiece respirators. - SARS-CoV-2 Infection and COVID-19 During Pregnancy: A Multidisciplinary Review. 5/30/2020. Narang K. Mayo Clin Proc.
A long summary: 15 pages. There’s obviously different physiology concerning gestation and pregnancy. Earlier reports suggest higher rates of preeclampsia and other pregnancy-related complications. Angiotensin-converting enzyme 2 receptor is upregulated in normal pregnancy. So, with higher ACE2 expression, pregnant women may be at elevated risk for complications from SARS-CoV-2 infection. Upon binding to ACE2, SARS-CoV-2 causes its downregulation, thus lowering angiotensin-(1-7) levels, which can mimic/worsen the vasoconstriction, inflammation, and pro-coagulopathic effects that occur in preeclampsia. Indeed, early reports suggest that, among other adverse outcomes, preeclampsia may be more common in pregnant women with COVID-19. - To Toci or Not to Toci for COVID-19: Is That Still the Question? 7/31/20. Cheng GS. Clin Infect Dis.
This is a very well written editorial describing the emergence of inflammatory inhibitors, such as tocilizumab, as potential treatment choices for COVID-19, and how the recent University of Michigan study adds credence to that choice.
August 5, 2020:
- COVID-19 Lung Injury and High-Altitude Pulmonary Edema. A False Equation with Dangerous Implications. 8/1/20. Luks AM. Ann Am Thorac Soc.
This is a well written opinion piece responding to the claim (now seen frequently on social media) that the pathophysiology of COVID pneumonia and high-altitude pulmonary edema (HAPE) are similar and may respond to similar therapies. The striking differences between the pathophysiologies of the two diseases are well described as are the expected responses of each to standard therapies for HAPE. The significant risk for adverse effects treating COVID pneumonia as HAPE are elucidated. - EDITORIAL: COVID-19: a complex multisystem disorder. 6/30/20. Roberts CM. Br J Anaesth.
COVID-19 has extensive effects on virtually all the organs. The virus binds to angiotensin converting enzyme 2 (ACE2) receptors present in vascular endothelial cells, lungs, heart, brain, kidneys, intestines, liver, pharynx, and other tissue. It can directly injure these organs. In addition, systemic disorders caused by the virus lead to organ malfunction. It can cause cytokine storm which can culminate in death. It causes inflammation, endotheliitis, vasoconstriction, hypercoagulability, and edema. Lymphocytopenia, elevated D-dimer, elevated fibrin degradation products (FDPs), and disseminated intravascular coagulation (DIC) are observed. Deep vein thrombosis (DVT), venous thromboembolism, pulmonary embolism (PE), systemic and pulmonary arterial thrombosis and embolism, and ischemic stroke are reported. In the heart, it can cause acute coronary syndrome, congestive heart failure, myocarditis, and arrhythmias. Kidney injury is usually secondary to systemic abnormalities. Stroke occurs even in young patients. Delirium and seizures are common. Anosmia and impaired sense of taste are reported. Psychological problems are common among patients as well as providers. Stool may contain virus. Lactate dehydrogenase may be elevated. Various skin manifestations including patchy erythematous rash are reported. Injury to an organ may become apparent long after the acute infection has subsided. Different organs may be affected at different times. Chronic injury may occur. Rehabilitation can be long and difficult. - Outcomes in COVID-19 Positive Neonates and Possibility of Viral Vertical Transmission: A Narrative Review. 8/1/20. Sheth S. Am J Perinatol.
This is an international review, mostly from China, of transmission from COVID-19 infected pregnant women to newborns. Of the 39 published reports, it includes only 326 COVID-19 positive women. Despite the small numbers, newborns were infrequently infected with COVID-19 at birth. Of the 23 COVID-19-positive neonates reported, no deaths resulted. - Prevalence and Impact of Myocardial Injury in Patients Hospitalized With COVID-19 Infection. 8/4/20. Lala A. JACC.
This is a retrospective analysis of troponin-I levels taken within 24 hours of admission from 2,736 patients admitted to Mount Sinai Health System hospitals between February 27 and April 12. Thirty-six percent of patients showed elevated levels (normal <0.03 ng/ml). After correction for co-morbidities and clinical severity, small elevations were associated with increased morbidity and mortality. Elevations greater than three times normal (>0.09ng/ml) were associated with significantly higher risk. Troponin may be a useful indicator of cardiac involvement and may aid disease stratification. - EDITORIAL: Myocardial Injury in COVID-19 Patients: The Beginning or the End? 8/1/20. Uriel N. J Am Coll Cardiol.
This editorial accompanies the article by Lala et al entitled, “Prevalence and Impact of Myocardial Injury in Patients Hospitalized with COVID-19 Infection,” and suggests pathophysiological pathways of cardiac involvement and underscores the importance of troponin-I elevations as markers of disease severity and outcome. The editorial reinforces the importance of cardiac involvement in COVID-19 disease and suggests troponin elevations could be a useful adjunct in disease stratification.
August 3, 2020:
- Association of Cardiac Infection With SARS-CoV-2 in Confirmed COVID-19 Autopsy Cases. 7/27/20. Lindner D. JAMA Cardiol.
Despite reports of fulminant myocarditis in patients with SARS-CoV-2 infection, this study of cardiac tissue from 39 consecutive autopsies of patients who died from confirmed disease demonstrates the presence of the virus in cardiac tissue but does not suggest an inflammatory reaction consistent with clinical myocarditis. The authors suggest further studies and clinical correlations are necessary to determine long-term consequences of SARS-CoV-2-specific myocardial infections. - Outcomes of Cardiovascular Magnetic Resonance Imaging in Patients Recently Recovered From Coronavirus Disease 2019 (COVID-19). 7/27/20. Puntmann VO. JAMA Cardiol.
This is a report of 100 cardiac magnetic resonance (CMR) imaging studies on recovered COVID-19 patients compared with 50 healthy age- and sex-matched controls and 50 risk-factor matched, non-COVID-19 patients. Seventy-eight percent of recovered patients had CMR abnormalities, while 60% had findings consistent with ongoing myocardial inflammation independent of preexisting conditions, disease severity and course of acute illness and recovery. Ongoing investigation is needed to determine course and long-term cardiac morbidity of COVID-19. - EDITORIAL: Coronavirus Disease 2019 (COVID-19) and the Heart-Is Heart Failure the Next Chapter? 7/27/20. Yancy CW. JAMA Cardiol.
This editorial raises the question of prevalence of cardiac involvement in COVID-19 disease and its impact on mortality and long-term morbidity. It discusses two relevant manuscripts and raises awareness of an important disease manifestation, the long-term implications of which are unknown and require investigation. - Characteristics and Strength of Evidence of COVID-19 Studies Registered on ClinicalTrials.gov. 7/27/20. Pundi K. JAMA Intern Med.
As an indication of how difficult it is to obtain quality data, this evaluation of 1,551 clinical studies of COVID-19 patients listed on ClinicalTrials.gov up to May 19, 2020 found that only 29.1% were designed in a way that the results could possibly change clinical practice (i.e., be classified as Level 2 evidence by the Oxford Centre for Evidence-Based Medicine level of evidence framework). In the 664 randomized clinical studies included, only 14% included mortality as a primary or composite outcome (arguably the most important research question). The authors state that, “Even before results are known, most studies likely will not yield meaningful scientific evidence at a time when rapid generation of high-quality knowledge is critical.” - Emerging pharmacological therapies for ARDS: COVID‑19 and beyond. 7/11/2020. Horie S. Intensive Care Med.
Members of the Regenerative Medicine Institute of the National University of Ireland authored this exhaustive overview of the current state of promising emerging pharmacological therapies of ARDS in patients with and without COVID-19. The review focuses on ongoing clinical and preclinical trials and uses well-designed tables and diagrams to enhance a complex array of pathophysiological mechanism and therapeutic interventions ranging from immune response modulation, to epithelial and endothelial integrity repair, anticoagulation and COVID-19 specific antiviral and anti-inflammatory therapies.
A valuable source, aimed at the research community, the authors express hope for identification of subtypes of ARDS and application to allow better targeting of specific therapeutic interventions in the future. - NIH Launches Platform to Serve as Depository for COVID-19 Medical Data. 7/29/20. Rubin R. JAMA.
Though not a research article, the news report, based on an NIH news release, summarizes an NIH effort to store and study medical record data from people across the country who have been diagnosed with coronavirus disease 2019. Certainly, research articles will be published in the future that will be based on this effort. For more information for institutions on how to contribute data, visit https://ncats.nih.gov/n3c/about/program-faq.
July 31, 2020:
- Age-Related Differences in Nasopharyngeal Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) Levels in Patients With Mild to Moderate Coronavirus Disease 2019 (COVID-19). 7/30/20. Heald-Sargent T. JAMA Pediatrics.
Although published only as a letter, the article contains timely data regarding the potential infectivity of children lacking significant symptoms. Nasal viral load as measured by nasopharyngeal swab PCR demonstrated higher levels in young children when compared to adults. At issue is that the study was performed in a pediatric center yet describes adult testing without elaborating how those samples were obtained. Timely article with the start of school approaching. - COVID-19 and thrombotic or thromboembolic disease: Implications for prevention, antithrombotic therapy, and follow-up. 6/16/20. Bikdeli B. J Am Coll Cardiol.
This article is an excellent clinically relevant review of thrombotic complications of COVID-19. Systemic and pulmonary venous and arterial thrombosis and thromboembolism are common in COVID-19. Thrombi are observed in virtually every organ. This is caused by inflammation, platelet activation, hypercoagulability, endothelial dysfunction, constriction of blood vessels, stasis, hypoxia, muscle immobilization, and disseminated intravascular coagulation (DIC).
Fever and inflammation cause hypercoagulability and impair fibrinolysis. Cytokine interleukin-6 (IL-6) levels correlate with hypercoagulability and disease severity.
Elevated antiphospholipid antibodies are associated with thrombosis. The liver increases production of procoagulant substances. Prothrombin time and activated partial thromboplastin time are moderately prolonged. Moderate thrombocytopenia is observed. C-reactive protein is elevated. Cytokine storm and excessive systemic inflammation are associated with lymphocytopenia, elevated D-dimer, elevated fibrin degradation products (FDP), and DIC. D-dimer levels and DIC are prognostic.
Guidelines recommend thromboprophylaxis. Prophylaxis with low-molecular weight or regular heparin, fondaparinux, or a direct oral anticoagulant such as apixaban or rivaroxaban should be considered. Heparins bind tightly to COVID-19 spike proteins impeding the entry of the virus into cells. Heparins also downregulate IL-6 and reduce immune activation. A non-randomized study suggests that among patients requiring mechanical ventilation, systemic anticoagulation may be associated with reduced mortality without increasing major bleeding. However, systemic anticoagulation has not proven to be beneficial in ARDS due to other etiologies. After hospital discharge prolonged prophylaxis may be beneficial. - COVID-19 pandemic and the skin: what should dermatologists know? 3/24/20. Darlenski R. Clin Dermatol.
Skin manifestations of COVID-19 are like those of other viruses and chronic inflammatory diseases like acne, eczema, psoriasis, and rosacea. Vascular problems associated with skin manifestations can be neurogenic, microthrombotic, or immune complex-mediated.
Of the patients with skin manifestations, a majority have patchy erythematous rash. Some have widespread urticaria or hives. A few also have chickenpox-like fluid-filled vesicles or blisters. They can have measles-like rashes. The most affected area is the trunk. Itching is mild or absent. Some patients have skin eruptions at symptom onset, and others after hospitalization. Lesions usually heal in a few days. Skin manifestations do not correlate with the severity of COVID-19.
Patients may develop livedo reticularis. It is a purplish net-like discoloration of the skin, often a result of blood clotting abnormalities. Lacy, dusky rashes, including dead skin cells are observed on the arms, legs, and buttocks. They are associated with hypercoagulability. Petechiae are present. Nonpruritic blanching livedoid vascular eruption, possibly due to vaso-occlusion may be present. They appear as mottled, netlike red or pink patches. Also present are chilblains, which are purplish, slightly firm and often tender. COVID toes and fingers have frostbite-like areas with red or purple rash or hive-like eruption. - Distinct clinical and immunological features of SARS-COV-2-induced multisystem inflammatory syndrome in children. 7/23/2020. Lee PY. J Clin Invest.
The authors retrospectively studied 28 confirmed cases of multisystem inflammatory syndrome in children at Boston Children’s Hospital from March to June 2020. Pediatric Multisystem Inflammatory Syndrome that includes classic features of Kawasaki disease, heterogeneous manifestations of systemic inflammation and shock. These children may exhibit heart failure, shock and coronary artery abnormalities, with a disproportionate representation among Blacks and Hispanics. Preexisting risk factors include obesity, asthma and heart disease. Acute respiratory distress syndrome was not a feature, but instead preponderance of cardiac complications including ventricular dysfunction and coronary abnormalities. The degree of inflammation as measured by CRP and procalcitonin is much greater in these children compared to those patients with COVID-19 pneumonia. Rapid diagnosis, multidisciplinary management and suppression of systemic inflammation was associated with a favorable outcome. - Genomewide association study of severe Covid-19 with respiratory failure. 6/17/20. Ellinghaus D. N Engl J Med.
Genetic differences may in part explain the difference in response of different persons to SARS-CoV-2. They compared hospitalized patients with respiratory failure with controls. They studied 835 patients and 1255 controls from Italy and 775 patients and 950 controls from Spain.
They found 3p21.31 gene cluster is a genetic susceptibility locus. Patients with blood group A were found to be at a higher risk of infection (odds ratio, 1.45) and develop more severe symptoms. Patients with blood type O were found to be at a lower risk of infection (odds ratio, 0.65). Although the results are statistically significant, the effect size is small. Results on the association with blood group has been reviewed by the SAB in several articles previously. - Prevalence of Gastrointestinal Symptoms and Fecal Viral Shedding in Patients With Coronavirus Disease 2019: A Systematic Review and Meta-analysis. 6/11/20. Parasa S. JAMA.
Gastrointestinal (GI) symptoms of COVID-19 include loss of appetite, nausea, vomiting, diarrhea, and abdominal discomfort. These symptoms might start before or occur with or without other symptoms such as fever, myalgias, and cough. Lower gastrointestinal tract is rich in ACE2 receptors.
About 40% of the patients’ stool tests positive for SARS-CoV-2 RNA. This is primarily due to RNA fragments of the virus. One study showed live virus on electron microscopy in a small percentage of patients. These patients’ stools are infectious. Patients who have virus in the stool take longer to clear it. Although a small percentage of patients have GI symptoms, up to one-half shed virus in the stool. Virus protein shell is also found in gastric, duodenal, and rectal cells.
More than one-half of COVID-19 hospitalized patients have elevated lactate dehydrogenase and other liver enzymes indicating injury to the liver or bile ducts. This is likely to be due to an overactive immune system or due to drugs causing liver damage. - Targets of T Cell Responses to SARS-CoV-2 Coronavirus in Humans with COVID-19 Disease and Unexposed Individuals. 5/15/20. Grifoni A. Cell.
To be effective, a COVID-19 vaccine has to elicit strong T cell immunity. Vaccines stimulate B cells to make antibodies against the virus. Helper T cells promote this. Those antibodies join with the virus, preventing it from entering a host cell and mark the virus for destruction. Once the virus infiltrates the host cell, antibodies are not effective. However, cytotoxic T cells can destroy infected host cells.
T cell immunity does not prevent re-infection but reduces the severity of symptoms. Among patients recovered from COVID-19, CD4+ T cells were observed in all and CD8+ T cells were observed in about 70%. CD4+ responses to spike antigen correlated with IgG and IgA antibody titers. Each of M, spike, and N antigens accounted for 11%–27% of the total CD4+ response. The remaining responses were against other SARS-CoV-2 antigens. This suggests that vaccines that target multiple antigens may be more effective than the ones targeting only the spike antigen.
T cell immunity is observed in persons infected and in about one-half of persons uninfected with SARS-CoV-2. The latter may have been previously infected with a virus such as one of the four human coronaviruses that cause colds. Thus, there is cross reactivity with other corona viruses. This may be a reason for variability in severity of clinical illness after infection.
Many of the vaccine candidates lead to production of the spike protein and antibodies against it. If the vaccine does not produce the spike protein with correct confirmation, the generated antibodies may be binding but not neutralizing antibodies. This can promote viral replication or form complexes that trigger more inflammation. Memory B and T cells that recognize the virus can provide protective immunity for years although the antibody titers may decline within months. Efforts are being made to genetically modify certain immune cells to target the virus.
July 29, 2020:
- Characterization of experimental and clinical bioaerosol generation during potential aerosol-generating procedures. 7/15/20. Doggett N. Chest.
This prospective study from Toronto quantified aerosol production pre and post two presumed aerosol generating procedures (AGPs); intubations in pigs (n=16) and elective bronchoscopies in human adults (n=39). Though overall, there was a significant reduction in larger particle aerosols during the procedures, and no significant increase in small particle aerosolization during the procedures, some bronchoscopies did produce significantly increased small particle aerosols. The authors conclude that the variability of aerosol generation reinforces the need for PPE during AGPs, and that more research is needed, especially in the more uncontrolled environments typical of a COVID-19 surge. - Considering the potential for an increase in chronic pain after the COVID-19 pandemic. 7/24/20. Clauw DJ. Pain.
An International panel reviews the underlying factors likely to lead to or exacerbate chronic pain in individuals during a pandemic whether or not an infection actually takes place. Addressing both chronic pain management professionals and acute care providers, this synopsis reminds us of post-SARS syndrome and urges us to prepare for post-COVID-symptomatology which includes chronic debilitating illnesses, like chronic fatigue, irritable bowel syndrome and interstitial cystitis and other conditions marked by a chronic pain experience. Registries, awareness and multidisciplinary teams will be required to deal with this likely scenario. - Remdesivir for Severe COVID-19 versus a Cohort Receiving Standard of Care. 7/25/20. Olender SA. Clin Infect Dis.
Pharma-sponsored proof of benefit of remdesivir in patients with severe COVID-19 is demonstrated by comparing patients’ clinical status on day 14 during two parallel studies. One is an international, 16-site retrospective cohort study of clinical outcomes in 800+ patients receiving standard-of-care treatment for severe COVID-19 infection; the other is an international, 45-center, phase 3, randomized, open-label trial comparing two courses of remdesivir in 312 patients. Remdesivir was associated with significantly greater recovery (74 vs 59%) and 62% reduced odds of death versus standard-of-care treatment. - Thrombosis in Hospitalized Patients With COVID-19 in a New York City Health System. 7/20/20. Bilaloglu S. JAMA.
This research letter reports retrospective data analysis from 3,334 consecutive hospitalized COVID-19 patients from four NYC hospitals. “Most” received low-dose thromboprophylaxis. Sixteen percent experienced thrombotic events defined as DVT, PE, MI, or CVA (no screening). ICU patients: 13.6% venous, 18.6% arterial. Ward points: 3.6% VTE, and 8.4% arterial. Mortality with event was 43% vs. 21% without. Age, male sex, Hispanic ethnicity, CAD, prior MI, and higher D-dimer at hospital presentation were associated with a thrombotic event, but not BMI or current smoking Hx.
July 27, 2020:
- A proposal for staging COVID-19 coagulopathy. 7/21/20. Thachil J. Res Pract Thromb Haemost.
Authors from three continents propose a framework within which to stage COVID-19 associated hemostatic abnormalities, and potentially guide treatment. A theory that infected lung epithelium acts as the epicenter of coagulation with early stages that are difficult to diagnose is described, along with a 3-stage disease model. Currently there are no reliable markers to guide treatment; however patterns and questions for researchers are outlined. A table outlines 11 current international clinical trials on approaches to coagulopathy and are listed on clinicaltrials.gov. - Design for Implementation of a System-Level ICU Pandemic Surge Staffing Plan. 7/23/20. Thakur N. Crit Care Explor.
Authors provide a comprehensive description of the design, dissemination, and implementation of an algorithm for multidisciplinary critical care staffing during surge demand, as implemented by a 40-hospital multi-state healthcare system. Staff is tiered according to skills and experience with team leadership roles for the most appropriate. On-site and telemedicine supervision are employed to optimally leverage oversight and scaling of patient loads. The plan provides for doubling of 750 ICU beds out of a total 5,500 beds. Consistent terminology and role-definition facilitate redeployment and allocation of human resources to meet changing local needs across diverse hospitals. - Inflammation Profiling of Critically Ill Coronavirus Disease 2019 Patients. 7/23/2020. Fraser DD. Crit Care Explor.
Report of a study comparing inflammatory profiling using multiple immunoassays between COVID-19 positive and negative ICU patients and a matched series of normal controls identifying a unique combination of six analytes distinguishing COVID-19 disease. Reported analytes were: tumor necrosis factor; granzyme B; heat shock protein 70; interleukin-18; interferon-gamma-inducible protein 10; and elastase 2.
Discussion notes COVID-19 patients demonstrate findings consistent with systemic inflammation including increased circulating cytokine levels and lymphopenia potentially characterizing the “purported” cytokine storm frequently mentioned.
Authors conclude: “In summary, we report sustained elevations in a unique combination of inflammatory analytes in COVID-19+ ICU patients. Our exploratory data are consistent with the slow, or absent improvement in COVID-19+ patients despite state-of-the-art ICU care, and could aid future hypothesis-driven research using larger ICU cohorts.” - Pulmonary embolism in hospitalised patients with COVID-19. 7/10/20. Whyte MB. Thromb Res.
A single center retrospective review of the results of 214 computer tomography pulmonary angiography studies performed on hospitalized Covid-19 patients with suspected pulmonary emboli. 31% of studies were positive for pulmonary emboli which represents 5.4% of all patients admitted during the study’s time interval. Elevated Wells score greater or equal to 4 did not predict results. Median D-dimer was 8000 ng/ml for patients with a positive study versus 2060 ng/ml for patients with a negative study, but low D-dimer had limited utility excluding patients with pulmonary emboli. - Pulmonary immune responses against SARS-CoV-2 infection: harmful or not? 7/19/20. Guillon A. Intensive Care Med.
A brief, well written review of the literature on COVID-19 immune responses claiming that the critical processes occur primarily in the lung and that the immune injury phase of the disease is not well described as a generalized “cytokine storm.” A T-cell subpopulation called innate T-cells appears to be diminished and have impaired function in peripheral blood but is found in increased numbers and activation in the airways of these patients. - Review of Viral Testing (Polymerase Chain Reaction) and Antibody/Serology Testing for Severe Acute Respiratory Syndrome-Coronavirus-2 for the Intensivist. 7/23/20. Motley MP. Crit Care Explor.
A nice review of nucleic acid amplification technology (PCR) and serological assays to diagnose, treat, and limit the spread of SARS-Cov-2 and it includes a discussion of the strengths and limitations of individual assays. - Strategies to Optimize ICU Liberation (A to F) Bundle Performance in Critically Ill Adults With Coronavirus Disease 2019. 7/23/20. Devlin JW. Crit Care Explor.
Multi-institutional panel reviews option to modify and apply the ICU Liberation Bundle to COVID-19 scenarios in the ICU. They strongly recommend applying the Bundle to effectively deal with pain, agitation and delirium wherever possible and offer a number of valuable suggestions, among those dealing with lack of resources, like PPE and utilizing non-critical care trained clinicians.
July 24, 2020:
- Blood type and outcomes in patients with COVID-19. 7/12/2020. Latz C. Ann Hematol.
Retrospective study of 1289 SARS-CoV-2 + patients /7648 tested patients w/ known ABO blood type. No blood group had an increased or decreased risk of severe disease, inflammatory markers, intubation, or death. Type A had the expected risk of +PCR, type A, type O had a lower risk and types B and AB and Rh+ patients had a higher risk. These results contrast w/ previous reports, however data are not fully comparable. - COVID-19 and the kidney: what we think we know so far and what we don’t. 7/22/20. Farouk SS. J Nephrol.
Review by the SAB
These authors are troubled by existing data related to true incidence, etiopathology, and its management with Covid-19. A heterogeneous report, with respect to population size, location, severity of illness, and definitions of acute kidney injury (AKI), show a wide range of rates of AKI occurrence in patients, from 1-46% and an equally wide percentage range of patients who were treated with kidney replacement therapy (KRT) (10-35%). Most patients with KRT were in the ICU (data was from the UK, Ireland, Italy, China, and the USA) and it has overwhelmed the nephrology services the world over. Potential explanations for these differences include the prevalence of co-morbid conditions and heterogeneity along racial and ethnic lines, local institutional policies about KRT timing, the use of extracorporeal KRT beyond classical “nephrological” indications. Using AKI as defined by “the 2019 Kidney Diseases: Improving Global Outcomes Consensus Conference” may standardize the whole process (a work in progress?). Mode of injury is also noted to be multifactorial. Though the link between AKI and poor outcomes is clear, prevalence and outcomes of COVID-19 in patients with chronic kidney disease and end-stage kidney disease has not yet been reported. In patients on immunosuppression like those with kidney transplants or glomerular disease, COVID-19 has presented a management dilemma. - Nutrition of the COVID-19 patient in the intensive care unit (ICU): a practical guidance. 7/19/20. Thibault R. Crit Care.
Review by the SAB
By Dr. Heinrich Wurm, on behalf of the SAB
French authors propose a flow chart and identify ten key issues for optimizing the nutrition management of COVID-19 patients in the ICU. Prominent among those is a preference for enteral nutrition whenever possible, attention to avoid the refeeding syndrome and awareness of the propofol infusion syndrome. Existing guidelines like GLIM* are valuable and their application encouraged. The use and limitations of indirect calorimetry during Covid-19 is discussed.
* Global Leadership Initiative on Malnutrition - Personalized Ventilation to Multiple Patients Using a Single Ventilator: Description and Proof of Concept. 7/17/20. Han JS. Crit Care Explor.
A proof of concept: the authors used components readily available in their hospital to assemble two “bag-in-a-box” breathing circuits. This shared ventilator function is proposed as a “last ditch” ventilatory assist device and not as a preferred ventilation mode. In a time of crisis where resources are limited, they introduced a system of multiple secondary breathing circuits driven by a ventilator in preference to that of simply splitting the breathing circuits. The authors hope, though, that this will not be needed. But these were all test conditions, not actually used on a patient. - Prospective study in 355 patients with suspected COVID-19 infection. Value of cough, subjective hyposmia, and hypogeusia. 7/21/20. Martin-Sanz E. Laryngoscope.
Review by the SAB
By Dr. Lance Lichtor, on behalf of the SAB
Of 355 patients who were healthcare personnel, there was a significant association between positive PCR and subjective hyposmia. If cough was added, the odds of having a positive RT-PCR increased significantly. The measurement of fever as the only method for screening of COVID-19 infection resulted in a poor association. - The role of chest radiography in confirming Covid-19 pneumonia. 7/18/2020. Cleverley J. BMJ.
An introductory summary of chest X-ray findings in COVID-19 pneumonia for the non-radiologist. Characteristic findings are illustrated however none is diagnostic. Studies show that X-ray imaging may initially appear normal or lag behind disease progression. Chest CT has been shown to be more sensitive however its initial use varies among countries. Includes no mention of chest ultrasound. - The Structural and Social Determinants of the Racial/Ethnic Disparities in the U.S. COVID-19 Pandemic: What’s Our Role? 7/17/20. Thakur N. Am J Respir Crit Care Med.
A call to arms for critical care and pulmonary specialists: black, Latinx, and Native Americans test positive for and die from coronavirus at higher proportion than other racial and ethnic groups. Their mortality rates far exceed the proportion of the population that these groups represent. Historically disadvantaged communities have reduced capacity to adopt preventive measures. Minority communities with low socioeconomic status (SES) and/or limited English proficiency receive less public communication during crisis and pandemics; access to testing and care is greatly limited in low-SES and minority communities. This article advocates for under-represented minority patients, who are becoming critically ill and dying at disproportionate rates.
July 22, 2020:
- Association Between Universal Masking in a Health Care System and SARS-CoV-2 Positivity Among Health Care Workers. 7/14/20. Wang X. JAMA.
This research letter from the Mass General Brigham healthcare system reports an association between the requirement for universal masking for their healthcare workers and a reduction in their percent positive COVID-19 PCR test results during a period of time when the disease continued to increase in the general population. The decrease in healthcare worker infections could have been confounded by other interventions inside and outside of the health care system, such as restrictions on elective procedures, social distancing measures, and increased masking in public spaces. However, the authors contend these results support universal masking as part of a multi-pronged infection reduction strategy in healthcare settings. - Dexamethasone in Hospitalized Patients with Covid-19 — Preliminary Report. 7/17/20. The RECOVERY Collaborative Group. N Engl J Med.
Review by the SAB
These authors (Nuffield /Oxford) provide preliminary results (recruitment ended on June 8) of the controlled, open-label-randomized evaluation of COVID-19 Therapy (RECOVERY) trial of dexamethasone in patients hospitalized with COVID-19. The primary outcome was mortality within 28 days after randomization.
In patients hospitalized with COVID-19, the use of dexamethasone (6mg either IV or PO up to 10 days) resulted in lower 28-day mortality among those who were receiving either invasive mechanical ventilation or oxygen alone at randomization but not among those receiving no respiratory support (may harm). In a 2:1 randomization, 2,104 patients received dexamethasone and 4,321 received the usual care. In the dexamethasone group, the incidence of death was lower than that in the usual care group among patients receiving invasive mechanical ventilation (29.3% vs. 41.4%; rate ratio, 0.64) and among those receiving oxygen without invasive mechanical ventilation (23.3% vs. 26.2%; rate ratio, 0.82). There was a trend showing the greatest absolute and proportional benefit among patients who were receiving invasive mechanical ventilation (11.5 by chi square test for trend). Patients in the dexamethasone group had a shorter duration of hospitalization than those in the usual care group (median, 12 days vs. 13 days) and a greater probability of discharge alive within 28 days (rate ratio, 1.10; 95%). It is likely that the beneficial effect of glucocorticoids in severe viral respiratory infections is dependent on a selection of the right dose, at the right time, in the right patient. Viral replication peaks in the second week of illness in SARS, while viral shedding in SARS-CoV-2 appears to be higher early in the illness and declines, thereafter when dexamethasone is most effective. At that stage, the disease may be dominated by immunopathological elements, with active viral replication playing a secondary role. - Excess Deaths From COVID-19 and Other Causes, March-April 2020. 7/1/20. Woolf, SH. JAMA.
The initial symptomatology, prodromal infective potential, anticipated course/severity, value of PPE and myriad additional variables were unknown when COVID-19 began its international journey. Early optimism in terms of containing and controlling the virus rapidly deteriorated as disease progression was recognized, the ability of asymptomatic carriers were known to be highly infectious and the initially unexpected benefit of universal face mask adoption created uncertainly about not only the viral spread but also the safety and reliability of the health system. Death is usually categorized accurately and reliable “death rate” statistics have been accumulated; the authors use seasonally adjusted U.S. death rates from December 29, 2013 to February 29, 2020 and compare historical to actual death rates reported between March 1, 2020 and April 2020 and include a secondary analysis in the five states most severely affected by the virus during the collection period. Careful data analysis was used to determine all-cause mortality and how COVID-19 influenced the total. The results attribute 65% of excess deaths to COVID-19-related causes and suggest that the total number is likely higher. Analysis was able to distinguish significant increases in other diseases during the period.
Also included is an insightful discussion underscoring importance of accurate determination of COVID-19’s true impact on not only death but also on hidden morbidity (including COVID-19 delayed treatment and/or resource constraints) which is still being elaborated. - EDITORIAL: Mortality and Morbidity: The Measure of a Pandemic. 7/1/20. Zylke JW. JAMA.
This editorial accompanying “Excess Deaths” further elaborates on the importance of, and difficulties associated with, estimating impact of COVID-19 on health systems and society. Peripheral effects are included and discussed. Together, the articles underscore the importance of classification and clarification in estimating disease impact, prevalence and spread in vulnerable populations and on society at large. - Hospitalization and Mortality among Black Patients and White Patients with Covid-19. 6/25/20. Price-Haywood EG. N Engl J Med.
Review by the SAB
By Heinrich Wurm, on behalf of the SAB
This retrospective cohort study takes a critical look at incidence, mortality and concomitant risk factors among black and white non-Hispanic members of the Ochsner integrated delivery health system.
Black patients far exceeded white non-Hispanics in getting infected (70 vs. 30% of enrolled patients were PCR positive), requiring hospital admission (77%) and dying (71%). But black race was not independently associated with a higher mortality (HR death vs. white race 0.89; 95 CI, 0.68-1.17) when adjustments for differences in socio-demographic and clinical characteristics were made.
Blacks had a greater prevalence of underlying disease (obesity, diabetes, hypertension, chronic kidney disease), presented with higher levels of inflammatory markers, elevated creatinine and were more likely to live in low-income areas and receive public insurance. Greater occupational exposure in service industries and higher incidence of morbid obesity and chronic kidney disease were also discussed. - Impact of delays on effectiveness of contact tracing strategies for COVID-19: a modelling study. 7/16/20. Kretzschmar ME. Lancet Public Health.
Review by the SAB
By Dr. Lance Lichtor, on behalf of the SAB
The authors used a mathematical model that describes the different steps of a symptomatic contact tracing strategy for COVID-19. They found reducing the testing delay (i.e., shortening the time between symptom onset and a positive test result, assuming immediate isolation) is the most important factor for improving contact tracing effectiveness. Reducing the tracing delay (i.e., shortening the time to trace contacts, assuming immediate testing and isolation if found positive) might further enhance contact tracing effectiveness, though this additional effect rapidly declines with increasing testing delay. - Neurobiology of COVID-19. 6/30/20. Fotuhi H. J Alzheimer’s Dis.
Review by the SAB
By Heinrich Wurm, on behalf of the SAB
This review by a panel of U.S. experts goes beyond analyzing neurological manifestations of COVID-19 and provides us with plausible and well-illustrated pathophysiological theories and a 3-stage evolution of a condition termed Neuro-COVID. A synopsis of worrisome post-COVID-19 neurological sequelae, ranging from poor memory and slow processing speed to lasting depression, Parkinson’s, multiple sclerosis and Alzheimer’s, concludes this remarkable publication and points us towards a future of COVID-related sequelae. - Outcomes from intensive care in patients with COVID‐19: a systematic review and meta‐analysis of observational studies. 6/30/20. Armstrong B. Anaesthesia.
Fascinating meta-analysis of 10,150 adult patients in 24 studies (enrollment was December 16, 2019 until May 28, 2020) from 11 countries with ICNARC (UK) database (national, rapidly updated registry) accounted for most cases in the study (results were unchanged when removed) with ICU death as primary endpoint. Mortality trended down from ~50% to 41.6% over time with confirmed by meta regression analysis by publication date indicating decreasing mortality. Discussion includes possibility of increasing sophistication of care outside ICU and despite likely increasing severity of ICU patients, therapeutic sophistication improvement was likely responsible for better outcome.
Excellent analysis with interesting discussion and conclusions emphasizing need for better national data reporting in real time to better follow disease progression and resource utilization. - Prevalence of SARS-CoV-2 in Spain (ENE-COVID): a nationwide, population-based seroepidemiological study. 7/6/20. Pollan M. Lancet.
Review by the SAB
By Dr. Robert Coffey, on behalf of the SAB
This article reports the results of antibody testing of 61,000 individuals across Spain, from April 27 to May 11, showing an overall national seropositive rate of only 5% (the majority of new diagnoses in Spain’s severe epidemic were made by May 1). Regions that experienced a more intense epidemic such as Madrid did have a seropositive rate of greater than 10%. Approximately one-third of the seropositive subjects reported having had no symptoms suggestive of COVID-19 infection. While specific locales such as Bergamo, Italy and some neighborhoods in Queens, NY may have seropositive rates high enough to confer local herd immunity, this does not seem to be occurring at a national level after severe epidemic episodes. - Race, Postoperative Complications, and Death in Apparently Healthy Children. 7/1/20. Nafiu OO. Pediatrics.
In a retrospective article of over 170,000 healthy children with care provided by anesthesiologists, African American children suffered more postsurgical complications, especially bleeding and death. - Redefining cardiac biomarkers in predicting mortality of inpatients with COVID-19. 7/17/2020. Qin JJ. Hypertension.
Detailed, retrospective analysis of available cardiac biomarkers of 3219 patients admitted to 9 hospitals in Hubei province between December 31st, 2019 and March 4th, 2020. Entry criteria included patients from 18 to 75 years old with documented COVID-19 on admission (RT-PCR and/or Chest CT) and high sensitivity cardiac troponin (hs-cTnI) or CKMB on admission with primary endpoint 28-day mortality. Statistical processing includes additional biomarker profiles, primary and secondary cardiac effects and analysis suggesting that in COVID-19 need to redefine reference range for Upper Limit of Normal to understand impact of cardiac effects.
The authors conclude “the abnormal cardiac biomarker pattern in COVID-19 patients was significantly associated with increased mortality risk, and the newly established COVID-19 prognostic cutoff values of hs-cTnI, CK-MB, (NT-pro)BNP, CK, and MYO were found to be much lower (~50%) than reference upper normal limits for the general population.” Valuable information that needs to be confirmed in different populations.
July 21, 2020:
- Pulmonary Angiopathy in Severe COVID-19: Physiologic, Imaging and Hematologic Observations. 7/15/20. Patel BV. Am J Respir Crit Care Med.
Describes standard and dual energy CT scan results in 39 consecutive Covid-19 pneumonia patients referred for ECMO care. The studies support the presence of pulmonary angiopathy with dilated peripheral vessels not typically seen in pulmonary emboli. No control studies were presented for comparison.
July 20, 2020:
- CPR in the COVID-19 Era – An Ethical Framework. 7/9/20. Kramer DB. N Engl J Med.
Review by the SAB
By David Clement, on behalf of the SAB
This opinion paper provides important reading on the ethics of how the surge of patients with COVID-19 complicate standard CPR practices. An ethical framework of three crisis standards is proposed: acknowledge resource limitations, forgo CPR in certain circumstances, and impose selective constraints on CPR to ensure the safety of healthcare personnel. Hospitals need to develop such explicit crisis standards for CPR to help clinicians and the public understand when strict adherence to established resuscitation protocols may no longer be appropriate. - Deep immune profiling of COVID-19 patients reveals distinct immunotypes with therapeutic implications. 7/15/20. Mathew D. Science.
Review by the SAB
By Dr. Uday Jain, on behalf of the SAB
Previously uncharted role of lymphocytes in COVID-19 is discussed. A wide variability in immune response was observed among hospitalized COVID-19 patients. Responses were barely detectable in about one-fifth of the patients. This was associated with pathology due to the virus and reduced survival. Remaining patients had CD8 and/or CD4 T lymphocyte and plasmablast responses that were heterogeneous among the patients and were divided into immunotypes. In many patients who became seriously ill with Covid-19, helper and killer cells do not work well cooperatively. An overabundance of helper cells is proinflammatory. An overabundance of killer T cells is not ideal but consistent with survival. - Individualizing Risk Prediction for Positive COVID-19 Testing: Results from 11,672 Patients. 6/20/20. Jehi L. Chest.
Review by the SAB
By Dr. Lance Lichtor, on behalf of the SAB
The authors of this article developed an online risk calculator that can identify individualized risk of a positive COVID-19 test. All patients from Cleveland Clinic in Ohio and Florida were tested, not just those who had the disease. Findings included: lower risk for Asians vs whites; lower risk for those who had pneumococcal polysaccharide vaccine and flu vaccine; higher risk with poor socioeconomic status; and reduced risk of testing positive in patients who were on melatonin, carvedilol, and paroxetine. - Protecting healthcare workers from SARS-CoV-2 infection: practical indications. 4/3/20. Ferioli M. Eur Respir Rev.
Review by the SAB
By Dr. Jay Przybylo, on behalf of the SAB
A “how to” based on oxygen therapy and dispersed exhaled breath. The importance of the article concerns exhaled breaths dispersion which depends on the mode of oxygen therapy. The remainder of the article is not scientifically based. - SARS-CoV-2 infection protects against rechallenge in rhesus macaques. 5/20/20. Chandrashekar A. Science.
Review by the SAB
By Dr. Uday Jain, on behalf of the SAB
Nine adult rhesus macaques infected with SARS-CoV-2 developed humoral and cellular immune responses leading to protective immunity. On re-challenge by SARS-CoV-2, there was a major attenuation of viral load in nasal mucosa and bronchoalveolar lavage in all of them. As the virus was still detectable, the protection was not sterilizing and the macaques could infect others. These results in primates suggest that patients who have COVID-19 may develop immunity to it. This is also essential for the development of a vaccine and determination of herd immunity. - The Impact of Coronavirus Disease 2019 Pandemic on U.S. and Canadian PICUs. 7/8/20. Sachdeva R. Pediatr Crit Care Med.
Review by the SAB
By Dr. Philip Lumb, on behalf of the SAB
This report is from a large pediatric ICU registry (Virtual Pediatric Systems, Los Angeles, CA), with data from over 200 hospital units and >1.5 million patient admissions. In order to determine the manner in which COVID-19 was affecting PICU’s, VPS expanded data collection related to COVID-19 to all Canadian and US PICU’s regardless of prior VPS membership to provide a near real-time dashboard including admissions, patient demographics and comorbidities, therapeutic interventions, deaths and length of stay. Data collection, from March 4 to May 20, represented 3,228 bed capacity comprising most US and Canadian resources from major teaching institutions to smaller hospitals with multifunctional PICU’s. At the peak of the admissions in late April, ~40% of admissions >18yo and ~12% >30yo indicating unusual age disparity than normally seen and providing insight into future PICU adjustments. Detailed description of analysis and future research directions are provided, demonstrating the value of high reliability registry with capability to provide rapid resource allocation and patient demographic, therapeutic and outcome information. - Therapeutic Plasma Exchange: A potential Management Strategy for Critically Ill COVID-19 Patients. 7/16/20. Tabibi S. J Intensive Care Med.
Review by the SAB
By Dr. Lydia Cassorla, on behalf of the SAB
This report briefly discusses various approaches currently being investigated to treat SARS-CoV-2 with a focus on potential benefits of therapeutic plasma exchange (TPE). TPE may alleviate the need for polypharmacy to combat various cytokines along with their associated side effects and necessary adjustments for comorbidities. TPE has been used to treat H1N1-associated ARDS, myasthenia gravis, Kawasaki disease, early septic shock, and various multi-organ dysfunction syndrome phenotypes including thrombocytopenia purpura. Reports of its use to treat severe COVID-19 are reviewed. TPE appears generally safe. Concerns involve blood supply, availability, and potentially cost. A proposed set of criteria that overlap with those for convalescent plasma and Spectra Optia Apheresis System is outlined, including early ARDS, severe disease, and life-threatening disease. Clinical trials are underway.
July 17, 2020:
- ABO Phenotype and Death in Critically Ill Patients with COVID-19. 7/1/20. Leaf RK. Br J Haematol.
Review by the SAB
By Lydia Cassorla, on behalf of the SAB
In this Letter to the Editor, ABO blood type data from adults admitted to ICUs over 38 days in the 67-center Study of the Treatment and Outcomes in critically ill Patients from COVID-19 (STOP-COVID) study were analyzed. Patients were followed until hospital discharge, death, or May 8, 2020 – a date that included a minimum of 28 days follow-up for those still hospitalized. 2033/3239 (62.8%) had ABO data available. 799/2033 (39.3%) died within 28 days. Death rates were similar across ABO phenotypes in all race/ethnicity categories, as well as Rh status. Among White patients, the observed distribution of ABO phenotypes differed from expected, primarily due to blood type A being over-represented (45.1% observed vs. 39.8% expected) and blood type O being under-represented (37.8% observed versus 45.2% expected). Among Black and Hispanic patients the observed and expected distributions of ABO phenotypes were similar. - An mRNA Vaccine against SARS-CoV-2 – Preliminary Report. 7/14/20. Jackson LA. N Engl J Med.
EDITORIAL: The Covid-19 Vaccine-Development Multiverse. 7/14/20. Heaton PM. Cardiovasc Res.
Review by the SAB
By Dr. David Clement, on behalf of the SAB
This paper and the associated editorial report the Phase 1 trial of a SARS-CoV-2 vaccine developed by the National Institute of Allergy and Infectious Disease and the private company, Moderna. In a dose escalation, 2 injection trial in 45 adults using a spike RNA viral antigen, the vaccine induced anti-SARS-CoV-2 immune responses in all participants, similar to the immune responses of recovered COVID-19 patients. Adverse events were common, but none were serious.
The accompanying editorial gives an overview of traditional vaccine development, how the current efforts have accelerated this usual process, and describes hurdles yet to be overcome. - COVID-19 Disease Severity Risk Factors for Pediatric Patients in Italy. 7/16/20. Bellino S. Pediatrics.
Review by the SAB
By Dr. Jay Pryzbylo, on behalf of the SAB
This large pediatric study demonstrates that infection by COVID-19 increases with age (severe illness in the youngest) is uncommon in the pediatric age group with only 1.8% of total infections over all ages. The study reported only 4 deaths, all in children with complex underlying medical issues. - Covid-19: What do we know about “long covid”? 7/14/20. Mahase E. BMJ.
Review by the SAB
By Dr. Barry Perlman, on behalf of the SAB
This non-peer reviewed article discusses “Long COVID,” a term used for lasting effects after recovering from COVID-19 infection or symptoms that persist longer than expected.
Ongoing health problems may include “breathing difficulties, enduring tiredness, reduced muscle function, impaired ability to perform vital everyday tasks, and mental health problems such as post-traumatic stress disorder, anxiety, and depression.”
HNS England will be launching an online portal for those with long-term effects of COVID-19 to communicate with nurses, physiotherapists, and mental health specialists.
A Facebook “long Covid Support group” has >7000 members, and the hashtag “longcovid” enables personal experiences to be shared on social media.
Research on the long-term effects of COVID-19 infection is needed. The Post-hospitalization COVID-19 Study plans to follow 10,000 UK patients for a year, but it will not include milder cases that didn’t require hospital care. - Neurological manifestations of COVID-19: a systematic review. 7/15/20. Nepal G. Crit Care.
Review by the SAB
By Dr. Heinrich Wurm, on behalf of the SAB
This well-organized review of the world literature up to May 20, 2020 analyses 37 articles, many of them case reports. The authors critically review each neurological symptom or disease entity currently known to exist with the intent to provide practitioners with an overview of a host of manifestations ranging from mild headaches to taste and smell disorders to strokes, hemorrhage and central and peripheral nervous system inflammatory reactions like encephalo-myelits and Guillain-Barré syndrome. - Palliative care for patients with severe covid-19. 7/14/20. Ting R. BMJ.
Review by the SAB
By Dr. Lance Lichtor, on behalf of the SAB
We usually think about a cure, but not everyone can be saved. This is a good article about managing patients with distressing symptoms, explaining the importance of having a strategy to manage patient deterioration and death, and stressing the importance of communication with the family with the sensitivity of noting that their loved one may soon die. - Relationship between ABO blood group distribution and clinical characteristics in patients with COVID-19. 6/21/20. Wu Y. Clin Chim Acta.
Review by the SAB
By Lydia Cassorla, on behalf of the SAB
Retrospective case controlled study of Wuhan patients admitted to a single Chinese hospital 1/20/20 – 3/5/20. 187 study patients were admitted with COVID-19 while 1991 control patients were COVID negative individuals admitted during the same time period. The proportion of patients with type A blood in the COVID-19 group was significantly higher than that in the control group (36.90% vs. 27.47%, P = 0.006), while the proportion of patients with type O blood in the COVID-19 group was significantly lower than that in the control group (21.92% vs. 30.19%, P = 0.018). Blood group A patients had a higher risk of COVID-19 than non-A blood group patients. (OR = 1.544, 95% CI = 1.122–2.104, P = 0.006). Blood group O patients had a lower risk of COVID-19 than non-O blood group patients (OR = 0.649, 95% CI = 0.457–0.927, P = 0.018).
July 15, 2020:
- Clinical Implications of SARS-CoV-2 Infection in the Viable Preterm Period. 7/3/20. Gulersen M. Am J Perinatol.
Review by the SAB
The authors in this article conducted a retrospective, logistic regression analysis for preterm birth (PTB) from boroughs in New York of patients diagnosed with COVID-19 infection with pregnancy between 23 and 37 weeks of gestation during March and April of 2020. PTB was noted to be in two groups: 23 to 33 weeks (n = 7/36) and the other one was 34+ (n = 18/29) with p= 0.0001. Most women with COVID-19 infection in the early preterm period recovered and were discharged home. The majority of PTB were indicated and not due to spontaneous preterm labor. Delivery during the current admission was noted as statistically significant for the group of patients with 34+ weeks. No correlation was noted with severity of the COVID-19 disease grade or treatment regimes (antibiotics and antimalarial) but no interleukins or steroids were given to the late group. Gestational age at diagnosis of COVID-19 infection had an odds ratio of 2.9. - Comparison of hydroxychloroquine, lopinavir/ritonavir, and standard of care in critically ill patients with SARS-CoV-2 pneumonia: an opportunistic retrospective analysis. 7/11/20. Lecronier M. Crit Care.
Review by the SAB
By Dr. Lance Lichtor, on behalf of the SAB
In critically ill patients admitted for SARS-CoV-2-related pneumonia, no difference was found between hydroxychloroquine or lopinavir/ritonavir as compared to patients who received standard of care only on the proportion of patients who needed treatment escalation at day 28. - Differential Ventilation Using Flow Control Valves as a Potential Bridge to Full Ventilatory Support during the COVID-19 Crisis: From Bench to Bedside. 7/2/20. Levin MA. Anesthesiology.
Review by the SAB
By Dr. Lance Lichtor, on behalf of the SAB
Proof of concept: single ventilator with split circuit. The author could increase one patient’s minute ventilation without affecting the other patient. Effective use for a crisis situation. The authors used custom-designed and manufactured flow control valves. - Factors affecting stability and infectivity of SARS-CoV-2. 7/6/20. Chan KH. J Hosp Infect.
Review by the SAB
Authors from a Chinese laboratory report the results of several (virus strain line, temperature, tissue infectivity dose, humidity, pH, etc.) experiments for the COVID-19 virus and its survival under different environmental situations. COVID-19 was able to retain viability for 3-5 days in dried form or 7 days in solution at room temperature, could be detected under a wide range of pH (2-13) conditions for several days and also 1-2 days in stool at room temperature but lost 5 logs infectivity. Common fixatives, nucleic acid extraction methods, and heat inactivation were found to significantly reduce viral infectivity. That will likely ensure hospital and laboratory safety during the COVID-19 pandemic but transmission related to food handlers and workers in meat and poultry processing facilities is possible. The presence of the virus on high-risk hospital surfaces should lead to concern about cleaning on other surfaces. It is estimated that 18% of infections are asymptomatic. With its propensity to cause milder infections, COVID-19 spreads more efficiently in communities in the absence of rigorous social distancing and environmental cleaning measures. - Is clinical effectiveness in the eye of the beholder during the COVID-19 pandemic? 7/9/20. Sandoval JL. BMJ Evid Based Med.
Review by the SAB
By Dr. Philip Lumb, on behalf of the SAB
Editorial noting the importance of maintaining clinical practice based on sound scientific evidence despite the current data overload from multiple poorly controlled or prematurely reported studies. Notes the importance of scientific balance in the media influenced public response to frequently incomplete, unsubstantiated, or erroneous data. - Risk factors for myocardial injury and death in patients with COVID-19: insights from a cohort study with chest computed tomography. 7/8/20. Ferrante G. Cardiovasc Res.
Review by the SAB
By Dr. Philip Lumb, on behalf of the SAB
Interesting study reporting admission CT Scan results on 332 consecutive patients with documented COVID-19 disease. Of these, 123 had myocardial injury defined as high-sensitivity troponin I above 20 ng/ml. Included patients had a median follow up of 12 days with 20.5% (68) deaths. Co-morbidities and course are well described; however, CT findings are consistent with lung involvement in COVID-19.
The study concludes that “myocardial injury, as assessed by cardiac troponins, occurs in approximately one third of COVID-19 cases and is associated with an adjusted two-fold mortality increase. An increased PA diameter, as assessed on chest CT, is an independent predictor of both myocardial injury and death.” - Tocilizumab for treatment of mechanically ventilated patients with COVID-19. 7/11/20. Somers EC. Clin Infect Dis.
Review by the SAB
By Dr. David Clement, on behalf of the SAB
An observational, controlled study of 154 adult, ventilated COVID-19 patients, half of whom received tocilizumab. Tocilizumab-treated patients had a 45% reduction in hazard of death, improved status on some secondary outcomes, and twice as many superinfections. Extensive tables, figures and statistical analysis provide insight. A randomized study is needed to confirm these findings.
July 14, 2020:
- Prevention of thrombotic risk in hospitalized patients with COVID-19 and hemostasis monitoring. 6/19/20. Susen S. Crit Care.
Review by the SAB
By Dr. Lydia Cassorla, on behalf of the SAB
Authors of this practical review article from a multinational European working group recommend a strategy to categorize thrombotic risk level and to increase anticoagulation above standard prophylactic doses for hospitalized COVID-19 patients with additional risk factors including obesity (BMI>30), respiratory failure, findings of major inflammation (D-dimer>3mcg/ml. or fibrinogen >8 g/L) or evidence of consumptive coagulopathy. They propose baseline testing repeated q48 hrs. and include a color-coded chart to quickly determine the risk category for individual patients. Not discussed: management of consumptive coagulopathy, thrombolysis, antiplatelet therapy, and arterial thrombosis. Their management strategy is based upon previously published international data.
July 13, 2020:
- Characteristics and serological patterns of COVID-19 convalescent plasma donors: optimal donors and timing of donation. 7/6/20. Li L. Transfusion.
Review by the SAB
By Dr. Barry Perlman, on behalf of the SAB
Study from Wuhan, China of 49 blood donors who recovered from mild-moderate COVID-19 to determine optimum convalescent plasma donor strategy.
Nucleocapsid (N) and Spike protein receptor-binding domain (S-RBD) antibodies were measured by ELISA assay. S-RBD ELISA results were correlated with a SARS-CoV-2 viral neutralization assay, as the authors state that recent studies suggest that S-RBD antibodies may provide immunity.
N specific IgM declined 3 weeks after infection and reached low levels after 6 weeks. S-RBD and N specific Ig G increased after 4 weeks from symptom onset.
Those who donated > 28 days from symptom onset, and whose fever > 38.5°C or lasted longer than 3 days, had higher levels of S-RBD IgG.
Further studies with larger sample size, plasma from asymptomatic donors, and clinical validation are needed. - COVID-19 Clinical Trials: Unravelling a Methodological Gordian Knot. 7/7/20. Mathioudakis AG. J Thromb Thrombolysis.
Review by the SAB
By Dr. Lance Lichtor, on behalf of the SAB
During a pandemic, in part because of the limit in a patient population that might shrink in the coming months, clinical trials might need to enroll a patient for more than 1 trial. In addition, because of the need to get information out quickly, interim data meta-analyses (or network meta-analyses) powered to evaluate key outcomes, may be useful. At least, strategies and methodologies need to be developed to allow the best use of data collected. - Extracorporeal Membrane Oxygenation During the Coronavirus 2019 Pandemic. 6/26/20. Mikkelsen ME. Crit Care Med.
Review by the SAB
By Dr. Jay Przybylo, on behalf of the SAB
An editorial addressing the use of ECMO in COVID-19 elaborating on an article describing ECMO for critically ill patients and demonstrating that survival was minimally better than conventional treatment of mechanical ventilation. - How to Quantify and Interpret Treatment Effects in Comparative Clinical Studies of COVID-19. 7/7/20. McCaw ZR. Ann Intern Med.
Review by the SAB
By Dr. Jay Pryzbylo, on behalf of the SAB
Concise but in depth explanation using the example of two previously published articles to demonstrate that the statistical techniques used do not necessarily accurately describe the outcomes achieved. At issue is that negative outcomes (e.g., deaths) are not adequately accounted for in positive outcome statistical evaluation (days to recovery). The authors advance a method to do so that alters the outcomes of the studies. - IS SURGICAL TRACHEOSTOMY BETTER THAN PERCUTANEOUS TRACHEOSTOMY IN COVID-19 POSITIVE PATIENTS? 7/2/20. Bassi M. Anesth Analg.
Review by the SAB
By Dr. Barry Perlman, on behalf of the SAB
Discussion of risks and benefits of percutaneous tracheostomy versus surgical tracheostomy, with strategies for safely performing percutaneous tracheostomies in COVID-19 settings. However, they recommend that a surgical tracheostomy is the first choice in the case of goiter, obesity, pneumomediastinum, difficult anatomy, coagulopathy, hemodynamic or respiratory instability. - Managing Anxiety in Anesthesiology and Intensive Care Providers during the Covid-19 Pandemic: An Analysis of the Psychosocial Response of a Front-Line Department. 7/8/20. Fleisher LA. NEJM Catalyst.
Review by the SAB
A survey about “anxiety / stress induced crisis of health care provider – HCP” conducted by Dr. Lee Fleisher of 242 MDs and CRNAs in the anesthesia and critical care medicine departments at University of Pennsylvania comes up with the best guidelines to follow for healthcare workers’ emotional well being during this pandemic.
Recommends:- Covid-19 Task Force
- Development of a protocol
- Simulation training
- PPE training for all – addressing comfort level.
- Communication through a town hall meeting regarding the root of anxiety, identification of symptoms (insomnia, appetite, living situation).
- Complementing weakness and strength of traits, culture, gender, experience, psychology, age-related burnout while addressing shared expertise of healthcare workers in the field.
Leadership should render the necessary training, psychological support, and clinical support, with acknowledgement of value of their work, to improve emotional health. The author stresses the role of meditation, maintaining routine including sleep, exercise, friends, and psychological assistance, and training.
- Thromboelastography Profiles of Critically Ill Patients With Coronavirus Disease 2019. 6/26/20. Yuriditsky E. Crit Care Med.
Review by the SAB
By Dr. Philip Lumb, on behalf of the SAB
Interesting retrospective study of 64 critically ill COVID-19 patients with available/reported thromboelastograph studies within 72 hours of ICU admission; 50% showed hypercoagulable profile defined as a Clotting Index (CI) >3. It is noted that D-Dimer > 2,000 ng/ml associated with median CI 3.4 while D-Dimer <2,000 ng/ml median CI 2.1. Discussion indicates TEG profiles consistent with fibrinogen and platelet effect and authors suggest further studies evaluating platelet aggregation profiles. While value of TEG evaluation in COVID-19 patients has not been confirmed, nonetheless further investigation is warranted as results consistent with clinical severity markers, D-Dimer elevations and requirements for appropriate and timely anticoagulation. - Treatment with Hydroxychloroquine, Azithromycin, and Combination in Patients Hospitalized with COVID-19. 6/29/20. Arshad S. Int J Infect Dis.
Review by the SAB
By Dr. Barry Perlman, on behalf of the SAB
Multi-center retrospective observational study of 2,541 consecutive RT-PCR confirmed COVID-19 admissions from March 10 to May 2 in Detroit to determine impact of hydroxychloroquine +- azithromycin on inpatient mortality.
Standard, uniform treatment guidelines established by a system-wide interdisciplinary COVID-19 task force also included corticosteroids and tocilizumab, which were used in 68% and 4.5% respectively.
In hospital mortality:- Overall 18%
- No hydroxychloroquine or azithromycin 26%
- Azithromycin alone 22%
- Hydroxychloroquine + azithromycin 20%
- Hydroxychloroquine alone 13.5%
- Mortality predictors were age > 65, CKD, decreased O2 sat on admit, ventilator use, and in contrast to previous studies, white race.
Propensity matched regression analysis showed a mortality hazard ratio of .49 for patients who received hydroxychloroquine.
Of note, no deaths due to major cardiac arrhythmias, such as torsades, were seen with hydroxychloroquine treatment.
The authors suggest that early medication treatment (91% within 48 hours of admission), standardized dosing, and inpatient telemetry with electrolyte protocols may have accounted for the positive results seen with hydroxychloroquine.
July 10, 2020:
- Critical Care Transesophageal Echocardiography in Patients during the COVID-19 Pandemic. July 1. Teran F. J Am Soc Echocardiogr.
This is a consensus statement from North American experts in TEE for emergency and critical care patients. There is a subset of intubated COVID-19 patients who may benefit from goal-directed TEE to gain information of immediate utility in determining clinical management. They emphasize pre-planning and individual assessment of who is likely to benefit when other POCUS is insufficient. - EDITORIAL: SARS-CoV-2 viral load and antibody responses: the case for convalescent plasma therapy. 7/8/20. Casadevall A. J Clin Invest.
Review by the SAB
By Dr. David Clement, on behalf of the SAB
Using a study on the kinetics of viral load and antibody response as an introduction, this article summarizes what is known about convalescent plasma therapy for COVID-19. The case is made for using sera from patients who recovered from severe COVID-19 disease (because of higher antibody titers), certainly giving therapeutic sera earlier (less than 10 days from symptom onset), and possibly giving therapeutic sera to patients with severe disease later in the course of their disease. - Improved Clinical Symptoms and Mortality on Severe/Critical COVID-19 Patients Utilizing Convalescent Plasma Transfusion. 6/23/20. Xia X. Blood.
Review by the SAB
By Dr. Lydia Cassorla, on behalf of the SAB
This article may be of interest to those looking to learn from the Chinese experience with convalescent plasma (CP). 138/1568 COVID-19 patients from this retrospective single-center Chinese cohort study received CP. Death (2.1% vs. 4.1%) and requirement for ICU care (2.4% vs. 5.1%) in the CP group were close to half of that in the untreated patients. Patients with higher initial lymphocyte counts and those who received CP treatment within 7 wks. from onset of clinical disease were more likely to respond. - Incidence of pulmonary embolism in non-critically ill COVID-19 patients. Predicting factors for a challenging diagnosis. 6/29/20. Mestre-Gómez B. J Thromb Thrombolysis.
Review by the SAB
By Dr. Barry Perlman, on behalf of the SAB
Retrospective review of EMR data of 452 consecutive patients admitted to the general ward with COVID-19 (based on WHO clinical criteria and/or RT-PCR) in Madrid to determine the incidence of PE in non-critically ill COVID-19 patients and identify predictive factors.- 91 of these patients had CT pulmonary angiography (CTPA) to rule out PE, with 29 (32%) positive for acute PE.
- Incidence of PE was 6.4% — 29/452 patients.
- Of note, 79% were receiving prophylactic LMWH at the time PE was diagnosed
- PE was not associated with a significantly increased risk of ICU admission or mortality
- Multivariate analysis showed lack of history of dyslipidemia and elevated D-dimer were independent predictors of PE.
- D-Dimer peak median was 2x higher in PE patients. Cut off predictor was > 5000 ug/dl.
- Patients with history of dyslipidemia had a 9x lower risk of PE. It is not known if this is due to statin use prior to admission. Hospital statin administration was not significantly different among the two groups.
While the study concludes that an elevated D-Dimer > 5000 ul/dl and lack of dyslipidemia history are independent predictors of COVID-19 related PE risk, it is limited by small sample size, retrospective nature, and lack of DVT studies.
- Rate of venous thromboembolism in a prospective all-comers cohort with COVID-19. 7/2/20. Rieder M. J Thromb Thrombolysis.
Review by the SAB
By Dr. Lydia Cassorla, on behalf of the SAB
This German prospective single-center study analyzed 190 ED patients with suspected COVID-19 March-April 2020. 49 SARS-CoV-2 positive (25.8%). 141 SARS-CoV-2-negative patients served as a control group. After 30-day follow-up, VTE was diagnosed in 3 SARS-CoV-2-positive patients (6.1%, including 2 ICU patients) vs. 5 SARS-CoV-2-negative (3.5%), however the difference was not statistically significant (p = 0.427). 30-day mortality was similar (6.1% vs. 5%, p = 0.720). COVID-19 disease severity correlated with the maximum D-dimer level during follow-up, but not D-dimer at admission.
Dyspnea was more common in the SARS-CoV2 negative group (41.7% vs. 52.4%, p = 0.002), whereas cough (58.3% vs. 37.6%, p < 0.0001) and fever (75% vs. 48.2%, p < 0.0001) were more frequent in COVID-19 patients. The rate of hospital admission was higher in the SARS-CoV-2 positive group (81.6% vs. 66.7%, p = 0.068) D-Dimers at admission did not differ between both groups (1.1 ± 1.4 mg/l vs. 0.8 ± 1.7 mg/l, p = 0.3). - Review of influenza-associated pulmonary aspergillosis in ICU patients and proposal for a case definition: an expert opinion. 6/22/20. Verweij PE. Intensive Care Med.
Review by the SAB
Although the number of COVID-19-associated aspergillosis (CAPA) cases that have been reported is a small number, in two series, similarities and differences with Influenza with Invasive Aspergillosis (IAP) and COVID-19 are pointed out. Here a group of authors (EU, USA and Taiwan) are seeking to change the definition of IAP (inclusive of clinical and radiological signs). They make a point that an under-estimation of IAP requires a need for vigilance for IAP in the ICU, an early diagnosis, holding steroids, judicious use of antiviral to avoid a fatal outcome due to an IAP patient in comparison to Influenza with IAP.
For CAPA:- 85% host factors are -ve but Lymphopenia/monocyte hyperimmune response is present
- IPA tracheobronchitis is not known
- The entry point ACE 2 – anti-fungal immunomodulation by antifungal not likely?
- Serum GM + ve – need a study in COVID-19 to understand the implication.
- No specificity of secondary infection organism types.
July 8, 2020:
- Anesthesiologists’ and intensive care providers’ exposure to COVID-19 infection in a New York City academic center: a prospective cohort study assessing symptoms and COVID-19 antibody testing. 6/11/20. Morcuende M. Anesth Analg.
Review by the SAB
By Dr. Heinrich Wurm, on behalf of the SAB
A prospective cohort study from Columbia University Irving Medical Center based on an email-based survey mailed on April 15, 2020. The survey asked for symptoms and COVID-19 antibody testing after work-related COVID-19 exposures, among anesthesiologists and critical care doctors in a large NYC academic medical center at the height of the pandemic.
The survey’s goal was to differentiate community from professional exposure and to evaluate the degree of protection PPE affords clinicians. The study achieved a 51% response rate and detected a 58% incidence of work-related exposure, 54% of which were high-risk exposures (e.g. intubation with inadequate PPE) and 26% reported symptoms suggesting COVID-19 infection.
Antibody testing revealed an almost identical 12% positive result among those with work-related exposure and those who did not report such an event. Antibody positive respondents were more likely to use NYC subway to commute to work and report COVID-19-like symptoms in the last 90 days. - Beyond the operating room: the roles of anaesthesiologists in pandemics. June 29. Ortega R. Br J Anaesth.
This is an interesting editorial that focuses on how historical cholera, polio and SARS epidemics redefined the role of anesthesiology, and how anesthesiologists in turn helped develop contact tracing, intensive care and infection control. The lessons learned from these previous epidemics provide guidance in the management of COVID-19 today. - Cardiopulmonary Resuscitation in Intensive Care Unit Patients With Coronavirus Disease 2019. 7/1/20. Cheruku S. J Cardiothorac Vasc Anesth.
Review by the SAB
By Dr. Philip Lumb, on behalf of the SAB
Interesting discussion involving practical, ethical and medical (physicians, ICU staff and ancillary personnel) decisions and preparations to perform cardiac resuscitation in terminally ill COVID-19 patients. Focuses on planning and preparing appropriate patients for potential resuscitation by informed discussion with patient/family, insertion of central venous access lines with long IV connections for access and infusion outside patient care area. CPR performed with automated chest compressor. Other safety elements described to protect staff and value of simulation in preparation emphasized. Novel approach to preparing for and performing CPR in COVID-19 patients. - Corrigendum to “Spinal anaesthesia for patients with coronavirus disease 2019 and possible transmission rates in anaesthetists: retrospective, single centre, observational cohort study” (Br J Anaesth 2020;124: 670-5). July 8. Zhong Q. Br J Anaesth.
- Spinal Anaesthesia for Patients with Coronavirus Disease 2019 and Possible Transmission Rates in Anaesthetists: Retrospective, Single-Centre, Observational Cohort Study Mar 28. Zhong. BJA.
COVID-19 SAB Opinion from: Dr. Jack Lance Lichtor
Spinal anesthesia was used for 49 patients who underwent mostly Caesarean section. For 7/49 patients, it wasn’t realized at the time that the patient had COVID-19 infection and the anesthesiologist used only level 1 protection; whereas level 3 protection was used for all other patients. For the anesthesiologists who used level 3 protection, 1 /37 developed COVID-19 infection compared with 4/7 who used only level 1 protection.
- Spinal Anaesthesia for Patients with Coronavirus Disease 2019 and Possible Transmission Rates in Anaesthetists: Retrospective, Single-Centre, Observational Cohort Study Mar 28. Zhong. BJA.
- Impact of SARS-CoV-2 Viral Load on Risk of Intubation and Mortality Among Hospitalized Patients with Coronavirus Disease 2019. 6/30/20. Magleby R. Clin Infect Dis.
Review by the SAB
By Dr. David Clement, on behalf of the SAB
This retrospective observational study of 678 inpatients in NYC shows that SARS-CoV-2 viral loads, as determined by cycle time (Ct) values of the RT-PCR test, are independently associated with intubation and death among hospitalized patients. This suggests that Ct values should be reported to assist clinicians in identifying patients at high risk for adverse COVID-19-related outcomes. - Long-Term ACE Inhibitor/ARB Use Is Associated with Severe Renal Dysfunction and Acute Kidney Injury in Patients with severe COVID-19: Results from a Referral Center Cohort in the North East of France. 7/5/20. Oussalah A. Clin Infect Dis.
Editorial: ACE inhibitors/ARB use and COVID-19. Time to change practice or keep gathering data?. 7/4/20. de Feria A. Clin Infect Dis.
Review by the SAB
By Dr. Heinrich Wurm, on behalf of the SAB
This well-designed retrospective longitudinal cohort study on patients admitted for severe COVID-19 to a tertiary referral university hospital in France finds that chronic ACE inhibitor and ARB use was associated with an increased risk of acute kidney injury as well as a potential interaction with the occurrence of acute respiratory failure. Although retrospective, this study stands out in its use of large amounts of high quality data and their sophisticated analysis allowing identification of potential groups of patients at higher risk for poor outcomes.
The accompanying editorial poses the question whether and when this and similar studies will impact clinical decision making. - Multisystem Inflammatory Syndrome in U.S. Children and Adolescents. 6/30/20. Feldstein LR. N Engl J Med.
Review by the SAB
By Dr. Jay Przybylo, on behalf of the SAB
One hundred eighty-six patients, up to 21 years old in age, were studied for COVID-19. GI symptoms were more common than respiratory. Only 8% demonstrated cardiac vessel abnormalities. Authors conclude this is not Kawasaki-related disease and thus label it MIS-C. - Original Article: Covid-19 Does Not Lead to a “Typical” Acute Respiratory Distress Syndrome. 3/30/20. Gattinoni. American Thoracic Society.
Review by the SAB
Excellent discussion based upon 16 ventilated COVID-19 patients that the virus does not cause a typical ARDS and these patients may benefit from low PEEP and prone positioning. - Reply to: Hedenstierna et al, Haouzi et al, Maley et al, Fowler et al, Bhatia and Mohammed, Bos, & Koumbourlis and Motoyama. 6/24/20. Gattinoni L. Am J Respir Crit Care Med.
Review by the SAB
By Dr. Barry Perlman, on behalf of the SAB
Response to correspondence regarding previously reviewed letter to the Am J Respir Crit Care Med by Gattinoni et al on COVID-19 and ARDS. The response reiterates two phenotypes of COVID-19 pneumonia:- Early L phenotype — atypical ARDS with lower elastance, lower Va/Q, lower recruit ability and lower lung weight.
- Late H phenotype — typical ARDS with higher elastance, higher R->L shunt, higher recruit ability, and higher lung weight.
They suggest the “contradictory results” reported by others may be due to the time of observation and reflect progression to the late H phenotype of the disease. They reiterate that the important feature of the L phenotype is not the high respiratory system compliance per se but the Va/Q mismatch induced hypoxia with a lung gas volume greater than is seen with ARDS “baby lung.”
They re-discuss mechanical ventilation management for the different phenotypes and suggest that the wide global disparity in COVID-19 ICU mortality rate may reflect the impact of “standard ARDS” treatment. - Revisiting the Protein C Pathway: An Opportunity for Adjunctive Intervention in COVID-19? 6/10/20. Mazzeffi M. Anesth Analg.
Review by the SAB
By Dr. Barry Perlman, on behalf of the SAB
Discussion of hypercoagulability in COVID-19 with a focus on the anticoagulant and anti-inflammatory properties of Protein C. The authors suggest that two modulators of the Protein C pathway — recombinant thrombomodulin and 3K3A-APC — may be beneficial in the treatment of severe COVID-19 as they are not associated with an increased risk of bleeding. - SARS-CoV-2-induced Acute Respiratory Distress Syndrome: Pulmonary Mechanics and Gas Exchange Abnormalities. 6/24/20. Barbeta E. Ann Am Thorac Soc.
Review by the SAB
By Dr. David Clement, on behalf of the SAB
This study from a single center in Spain describes in detail the gas exchange, pulmonary mechanics and ventilatory management of 50 consecutive ventilated patients with COVID-19 ARDS. On average, COVID-19 patients had a similar presentation as non-COVID-19 ARDS patients, though pulmonary compliance was remarkably more heterogeneous in those with COVID-19. Several tables and figures displaying physiologic data will be of interest to critical care physicians caring for COVID-19 ARDS. - Severe Acute Respiratory Syndrome Coronavirus-2 Cardiovascular Complications: Implications for Cardiothoracic Anesthesiology. July 1. Cormican DS. J Cardiothorac Vasc Anesth.
Review of pathophysiology and clinical effects of SARS-Cov-2 infection on cardiac function and supportive and interventional therapeutic options available. Good discussion and review of topic and current information available to date.
July 6, 2020:
- Compassionate Use of Tocilizumab for Treatment of SARS-CoV-2 Pneumonia. 6/23/20. Jordan SC. Clin Infect Dis.
Review by the SAB
By Dr. Heinrich Wurm, on behalf of the SAB
Single center review by a multidisciplinary team from Cedars-Sinai following 27, mostly intubated, patients with confirmed SARS-CoV-2 pneumonia who received a single dose of 400 mg tocilizumab intravenously under a compassionate use protocol. Decreasing vasopressor support and oxygen requirements as well as lower C-reactive protein levels and temperature were observed in a majority of subjects monitored to assess anti-inflammatory effectiveness and clinical improvement.
Tocilizumab proved beneficial in reducing inflammation and improving clinical outcome including mortality. Final proof of the drug’s efficacy awaits a placebo-controlled trial, now underway. - Drug-Induced Liver Injury and COVID-19 Infection: The Rules Remain the Same. 6/8/20. Olry A. Drug Saf.
Review by the SAB
By Dr. Philip Lumb, on behalf of the SAB
Editorial noting that patients have been discontinued/withdrawn from studies because of suspected drug-induced liver damage that does not meet international guidelines for association. A summary of currently used drugs in COVID-19 and possible interactions that may cause liver damage is listed. However, the authors state that since many drugs used in therapeutic interventions may be related to liver damage, it is important to discuss acute liver injury on internationally defined biologic criteria “on the Upper Limit of Normal of serum alanine aminotransferase activity (ALT), serum alkaline phosphatase activity (ALP) and serum concentration of total bilirubin,” which are provided in the editorial as well as a severity grading score to include in association. Internationally recognized criteria for DILI should be satisfied to confirm the diagnosis prior to premature removal of patients from potentially important clinical trials. - Extracorporeal Membrane Oxygenation for Critically Ill Patients with COVID-19 Related Acute Respiratory Distress Syndrome: Worth the Effort? 6/16/20. Falcoz PE. Am J Respir Crit Care Med.
Review by the SAB
By Dr. David Clement, on behalf of the SAB
A prospective, single-center study from France following 17 COVID-19 patients who met defined criteria and were placed on ECMO. The endpoints at 60 days were death (6 patients, 35%), discharge from hospital (9 patients, 41%), inpatients off the ventilator (3 patients, 17%) and still ventilated (1 patient, 6%). Nearly half of the patients had major bleeding or thrombotic complications. The authors conclude that “Considering the high frequency of severe adverse events, ECMO should probably remain a rescue therapy and therefore be undertaken only in ECMO-expert centers with adequate resources.” - Inhalational volatile-based sedation for COVID-19 pneumonia and ARDS. 6/25/20. Jerath A. Intensive Care Med.
Review by the SAB
By Dr. Heinrich Wurm, on behalf of the SAB
In light of a growing shortage of sedatives and intravenous anesthetics, this narrative review from Toronto highlights the benefits and technical details of volatile anesthetics for sedation in the critical care unit during the COVID-19 pandemic.
Spearheaded in Europe – volatile anesthetics using in-line vaporizers may provide added benefits, like bronchodilatation and an anti-inflammatory effect, but safe use requires trained teams familiar with volatile anesthetics administration in the ICU. The authors provide a comprehensive and realistic review of available options and alternatives.
July 1, 2020:
- COVID and Coagulation: Bleeding and Thrombotic Manifestations of SARS-CoV2 Infection. 6/3/20. Al-Samkari H. Blood.
Review by the SAB
This is a retrospective observational study of data from 400 COVID-19 in-patients with D-dimer on admission to 5 affiliated Boston area hospitals between March 1 – April 5, 2020 with a data cutoff of April 8, 2020. All received prophylactic anticoagulation except one who was fully anticoagulated. Incidence of thrombosis and bleeding was similar to that reported in non-COVID-19 patients with equivalent illness severity. (9.5% had thrombosis and 4.8% hemorrhage w/ higher fractions in the critically ill.) There were no deaths from thrombosis and 1 from intracerebral hemorrhage. D-dimer on admission was predictive of thrombosis, bleeding, illness severity and death. The authors recommend that clinicians await the results of randomized clinical trials before increasing thromboprophylaxis dosages for COVID-19 patients, including the critically ill. - Prevention, diagnosis and treatment of venous thromboembolism in patients with COVID-19: CHEST Guideline and Expert Panel Report. 5/26/20. Moores LK. Chest.
Review by the SAB
By Dr. Jay Przybylo, on behalf of the SAB
The vast majority of data over the years support combination antiplatelet and anticoagulant prophylaxis. In summary, this is a very important document that will be used by the medical authorities, the legal profession, hospitals, and societies to be a reference for clinical behavior. - The association of lung ultrasound images with COVID-19 infection in an emergency room cohort. 6/11/20. Bar S. Anaesthesia.
Review by the SAB
For emergency room patients with suspected COVID-19 disease, the delay in RT-PCR testing results can cause unnecessary isolation of patients and a strain on hospital resources. This prospective study of 100 ER patients from France found that a POCUS protocol (BLUE) in conjunction with the quick SOFA score accurately predicted RT-PCR positive patients and worse outcomes.
International Anesthesia Research Society
